When considering dental implants, one significant challenge can be the presence of soft bone tissue, which may not adequately support the implant. Soft bone conditions, typically resulting from factors like osteoporosis, periodontal disease, or long-term tooth loss, require specialized treatment approaches. This article explains various techniques and advancements in implantology aimed at overcoming these challenges. From bone grafting to innovative implant designs, learn about the various strategies that can improve treatment outcomes and ensure the longevity of dental implants even in patients with less dense bone structure.
Understanding Dental Implants in Soft Bone
Dental implants have revolutionized the field of dentistry, providing a reliable solution for tooth replacement that mimics natural teeth in functionality and aesthetics. However, one of the significant challenges dentists face is dealing with soft bone. Understanding the intricacies of soft bone is crucial for the successful placement and longevity of dental implants.
In this article, we will explore the nature of soft bone, its impact on dental implants, and the diagnostic methods used to assess it. This knowledge is essential for both dental professionals and patients to make informed decisions regarding implant procedures.
What is Soft Bone?
Soft bone, also known as low-density bone or Type IV bone, is characterized by its lower mineral content and porous structure. This type of bone has less trabecular density compared to harder bones, making it more flexible and less capable of supporting heavy loads.
Bone density varies significantly among individuals and can also be influenced by factors such as age, gender, and underlying health conditions. Bones in the posterior maxilla, for example, are commonly softer due to lower mechanical stress in that region.
Several factors, including osteoporosis, long-term steroid use, and certain metabolic disorders, can contribute to reduced bone density. Understanding these contributing factors is essential for planning successful dental implant treatments in patients with soft bone.
How Soft Bone Affects Dental Implants
The success of a dental implant largely depends on its stability, which is initially mechanical and later biological through a process called osseointegration. Soft bone presents a challenge for mechanical stability due to its porosity and reduced density, leading to a higher risk of implant failure.
Several studies have shown that implants placed in soft bone regions have a higher incidence of micromovement during the healing phase. This micromovement can disrupt the formation of a stable bone-implant interface, potentially leading to implant looseness and failure.
To address these challenges, various techniques have been developed, including the use of shorter or wider implants, bone grafting, and guided bone regeneration (GBR). These methods aim to enhance the bone quality and provide a more stable foundation for the implants.
Diagnostic Methods for Soft Bone
Accurate diagnosis of bone quality is a critical step in the dental implant planning process. Several diagnostic tools and techniques are employed to evaluate bone density and structure before placing an implant.
Cone Beam Computed Tomography (CBCT) is one of the most advanced imaging techniques used to assess bone quality. It provides detailed 3D images that allow clinicians to evaluate the bone’s density, volume, and anatomical structures surrounding the implant site.
- Dual-energy X-ray absorptiometry (DEXA): Commonly used to measure overall bone density, DEXA can provide crucial insights into a patient’s general bone health.
- Intraoral radiographs: These are helpful for preliminary assessments but offer limited information compared to CBCT and DEXA.
- Clinical evaluation: A tactile assessment using a dental probe during surgery can provide immediate feedback on bone quality at the implant site.
Through these diagnostic methods, clinicians can develop a comprehensive treatment plan tailored to the specific bone quality of each patient, thereby increasing the likelihood of successful implant integration.
Understanding the nuances of dental implants in soft bone is just the beginning. For more in-depth knowledge, explore our other articles that cover various aspects of implantology and bone regeneration techniques.
Challenges of Dental Implants in Soft Bone
When it comes to dental implants, one of the primary challenges is dealing with soft bone tissue. Soft bone, often found in the posterior regions of the upper jaw, presents unique difficulties that can affect the success of the implant procedure. Ensuring the long-term stability and functionality of implants in these regions requires specialized techniques and a deep understanding of the underlying biological processes. Soft bone tissue is characterized by its lower density and reduced mineral content compared to harder bone regions. This makes it more prone to resorption and less capable of providing the immediate stability needed for implant support. Consequently, dental professionals need to adopt advanced methods to enhance the bone quality and secure reliable implant fixation in such conditions.
Various strategies, such as bone grafting, sinus lifts, and the use of specialized implant designs, have been developed to address the challenges posed by soft bone. These interventions aim to improve bone volume and quality, offering a more stable foundation for the dental implants. Despite these advances, practitioners must remain vigilant to identify and mitigate the potential complications associated with soft bone implant procedures.
Common Issues Faced
One of the most common issues encountered when placing dental implants in soft bone is the poor primary stability of the implant. Because soft bone does not provide the same level of resistance as dense bone, there is a higher risk of micromovements occurring during the healing period. These micromovements can disrupt the osseointegration process, leading to implant failure.
Additionally, the rate of bone resorption tends to be higher in soft bone areas. This can result in a gradual loss of bone around the implant, compromising its long-term stability and functionality. To counteract this, strategies such as using wider or longer implants, and immediate loading protocols are often implemented.
Another issue is the elevated risk of peri-implantitis, an inflammatory condition affecting the tissues surrounding the implant. Soft bone areas are more susceptible to bacterial colonization, which can lead to infection and inflammation. Meticulous oral hygiene and regular follow-up appointments are essential to monitor and manage this risk effectively.
Moreover, achieving adequate aesthetic outcomes can be more challenging in soft bone regions due to the potential for bone resorption and soft tissue recession. This could affect the overall appearance and satisfaction of the patient, necessitating additional procedures such as soft tissue grafting to enhance the aesthetic results.
To explore more about overcoming these challenges and achieving successful dental implant outcomes, stay tuned for our upcoming articles on advanced implantology techniques and innovations in bone regeneration.
Solutions for Dental Implants in Soft Bone
Dental implants have revolutionized restorative dentistry, offering a permanent solution for missing teeth. However, implant placement in soft bone presents unique challenges that require specialized techniques and approaches. This article explores different solutions aimed at improving implant success rates in soft bone conditions.
Understanding the factors that affect implant stability in soft bone is crucial. Soft bone, often characterized by low density and poor quality, can hinder the osseointegration process, leading to potential implant failure. Innovations in bone grafting techniques, implant design modifications, and post-operative care are essential to addressing these challenges effectively.
Bone Grafting Techniques
Bone grafting is a common procedure to augment the bone volume and density before implant placement. It involves transplanting bone tissue to the deficient area, promoting new bone growth and improving the structural integrity of the implant site. Several grafting techniques have been developed to enhance outcomes in soft bone scenarios.
There are various types of bone grafts used in dentistry:
- Autografts: Harvested from the patient’s own body, offering a high success rate due to biological compatibility.
- Allografts: Derived from human donors, processed to ensure safety and effectiveness.
- Xenografts: Sourced from animals, often bovine, and treated to be biocompatible.
- Alloplasts: Synthetic materials mimicking the properties of natural bone.
Each type of graft has its advantages and limitations. Autografts are considered the gold standard but require a secondary surgical site. Allografts and xenografts eliminate the need for a donor site but vary in integration rates. Alloplasts offer a synthetic alternative but may require longer healing periods.
Implant Design Modifications
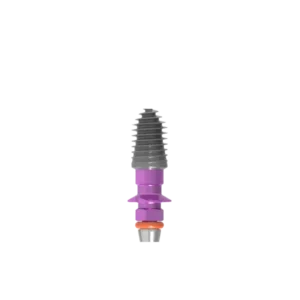
Advancements in implant design have significantly improved the success rates in soft bone conditions. Modifications in implant surface texture, shape, and material can enhance stability and osseointegration. For instance, implants with a roughened surface promote faster bone cell adhesion compared to smooth surfaces.
Conical or tapered implants are particularly beneficial in soft bone as they mimic the natural tooth root shape, providing better distribution of occlusal forces. This design minimizes micro-movements, reducing the risk of implant failure. Additionally, shorter implants with a wider diameter are often preferred to maximize contact with the available bone.
Implant materials also play a critical role. Titanium remains the material of choice due to its excellent biocompatibility and mechanical properties. However, newer materials like zirconia are gaining popularity for their aesthetic benefits and strong osseointegration capabilities with soft bone.
Post-Operative Care and Monitoring
The success of dental implants in soft bone not only relies on surgical techniques and implant design but also on meticulous post-operative care and monitoring. Immediate post-surgery care includes managing inflammation, ensuring proper oral hygiene, and avoiding undue stress on the implant site.
Regular follow-up appointments are essential to monitor healing and detect any signs of complications early. Radiographic imaging helps in assessing bone regeneration around the implant and identifying issues such as insufficient osseointegration or peri-implantitis.
Patients are advised to follow specific instructions to maintain implant health:
- Maintain rigorous oral hygiene to prevent infections.
- Avoid smoking, as it can impede healing and increase the risk of implant failure.
- Adhere to a soft diet initially to minimize pressure on the implant site.
- Report any unusual symptoms such as pain or mobility of the implant.
In conclusion, using a combination of advanced bone grafting techniques, strategic implant design, and diligent post-operative care can significantly enhance the success of dental implants in soft bone conditions. For more insights into implantology and regenerative treatments, explore our other articles on cutting-edge dental solutions.
Frequently Asked Questions About Dental Implants with Soft Bone
Understanding the challenges and solutions involved in dental implants with soft bone can help patients make informed decisions about their oral health. Here are some commonly asked questions about this topic.
What are the main challenges of placing dental implants in soft bone?
The main challenges include insufficient bone density which can lead to poor implant stability and a higher risk of implant failure. Soft bone may not adequately support the implant, necessitating additional procedures such as bone grafting to enhance the bone quality and ensure the longevity of the implant.

My name is Salman Kapa, a 73-year-old expert in bone regeneration and dental implantology. With decades of experience in the field, I am dedicated to advancing our understanding of oral health and hygiene. Through my research and writing, I aim to contribute to the development of innovative solutions in dental care.