Bone grafting for implants is a crucial procedure for those who lack sufficient jawbone density to support dental implants. The process involves transplanting bone tissue to the jawbone, promoting growth and providing a stable base for the implant. This not only enhances the structural integrity of the jaw but also ensures the longevity and functionality of the dental implants. Understanding the variety of bone graft materials and techniques can help patients make informed decisions about their dental health.
What is Bone Grafting?
Bone grafting is a crucial procedure in the field of dental implantology and regeneration. This technique involves the transplantation of bone tissue, which can facilitate the integration of dental implants by providing a solid foundation where there might be insufficient natural bone. The success of dental implants often hinges on the quality and quantity of the underlying bone, making bone grafting an indispensable step for many patients.
The process of bone grafting is tailored to address specific needs, ensuring that the optimally prepared site is available for implant placement. Different methods and materials are employed depending on the individual case requirements. Understanding the various aspects of bone grafting helps in comprehending its importance in achieving long-term stability and functionality of dental implants.
Definition and Purpose
Bone grafting is defined as the surgical procedure that replaces missing bone in order to repair bone fractures that are extremely complex, pose a significant health risk to the patient, or fail to heal properly. In dental implantology, the purpose of bone grafting is to create a sufficiently robust and dense bone structure that can support the placement and stability of dental implants.
The primary purpose of bone grafting in dental implantology can be summarized as follows:
- Enhancing bone volume: This is crucial for sites with insufficient bone mass to support implants.
- Facilitating osseointegration: Proper bone structure ensures that the implant integrates well with the natural bone.
- Restoring facial aesthetics: Bone grafting can help in maintaining or restoring the natural contours of the jawbone.
Types of Bone Grafts
There are several types of bone grafts used in dental procedures, each with its own set of advantages and applications. The choice of graft depends on the patient’s specific needs, the extent of bone loss, and the location of the implant. The main types of bone grafts are:
- Autografts: Tissue harvested from another part of the patient’s own body. This is considered the gold standard as it carries no risk of rejection.
- Allografts: Bone sourced from donor tissue, typically obtained from a bone bank. These are thoroughly processed to ensure safety.
- Xenografts: Bone derived from another species, usually bovine. These grafts are treated to prevent immune rejection.
- Alloplastic grafts: Synthetic materials such as hydroxyapatite or tricalcium phosphate, which are biocompatible and encourage bone growth.
Each type of graft has its indications and is chosen based on factors like the size of the defect, the patient’s health condition, and specific requirements for healing and integration.
Candidates for Bone Grafting
Not every patient requires bone grafting for dental implants. However, there are specific conditions that necessitate this procedure. Ideal candidates for bone grafting include those who:
- Have significant bone loss due to periodontal disease, trauma, or previous tooth extractions.
- Require dental implants but lack sufficient bone mass to support them.
- Experience jawbone atrophy over time, which can result from long-term denture use.
- Need ridge augmentation to restore the natural contour of the gums and jaw.
Overall health, including non-smoking status and no chronic conditions like diabetes, which can impair healing, are factors also considered when determining eligibility for bone grafting. Consulting with a dental specialist will help in understanding the necessity and planning the appropriate treatment approach.
By gaining deeper insights into bone grafting, patients can better appreciate the complexities and benefits of this procedure. For more information on related topics, consider reading our other articles on dental implantology and bone regeneration techniques.
The Bone Grafting Procedure
Pre-Procedure Preparation
Preparation for a bone grafting procedure is critical for ensuring optimal outcomes and minimizing complications. Initially, a comprehensive evaluation of the patient’s oral health is performed, including checking for any pre-existing conditions such as periodontitis or systemic diseases that may affect healing. A detailed medical history is reviewed to identify any contraindications for the procedure.
Imaging studies such as CT scans or cone-beam computed tomography (CBCT) are essential to assess the thickness of the patient’s cortical bone and to determine the shape of the residual ridge. This enables the dentist to plan the grafting procedure with precision. Often, a surgical guide is prepared based on these imaging studies to aid in the accurate placement of the grafting material.
Patients are also advised to cease smoking and follow a balanced diet rich in vitamins and minerals to enhance healing. Antibiotics and antiseptic rinses may be prescribed pre-operatively to minimize the risk of infection. Ensuring that the patient is in optimal health before starting the procedure significantly boosts the success rate of bone grafting.
Step-by-Step Process
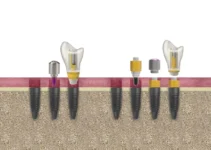
The bone grafting process begins with the administration of local anesthesia to ensure the patient’s comfort. A precise incision is then made to expose the area requiring the graft. If there is insufficient bone, autologous bone (bone harvested from the patient) is often used, either alone or in combination with a biomaterial such as hydroxyapatite or tricalcium phosphate.
In such cases, the graft material is strategically layered to correct any deficiencies, often overcorrecting by 1 or 2 millimeters to account for resorption during the remodeling phase. The biomaterial serves as a scaffold, promoting new bone growth while maintaining the shape of the graft site.
The graft is then covered with a thin membrane, ensuring it stays in place and is protected during the healing process. The membrane should be thin to allow for adequate vascularization, which is critical for the integration of the graft with the existing bone.
Finally, the surgical site is sutured, and a protective dressing is applied. Patients are instructed to follow specific postoperative guidelines to ensure the success of the graft.
Post-Procedure Care
After the bone grafting procedure, postoperative care is crucial to ensure successful healing and integration of the graft. Patients are typically prescribed pain relievers and antibiotics to manage discomfort and prevent infection. It’s essential to maintain good oral hygiene without disturbing the surgical site; using an antiseptic mouth rinse can help.
Swelling is a common occurrence and can be managed with cold compresses and keeping the head elevated. Patients should avoid hard or crunchy foods and opt for a soft diet for at least a week following the procedure. Regular follow-up appointments are necessary to monitor the healing process and address any concerns promptly. It’s also vital for patients to avoid smoking and limit alcohol consumption as these can significantly impair the healing process. Adhering to these guidelines ensures that the bone graft integrates successfully and provides a strong foundation for future dental implants.
For further reading on similar topics, be sure to check out our other articles on dental implantology and regenerative techniques.
Recovery After Bone Grafting
Bone grafting is a critical procedure in implantology and oral regeneration, designed to provide a solid foundation for dental implants. Post-surgical recovery is a vital phase that significantly impacts the success of the graft and the overall outcome of the procedure. Proper care and awareness about potential complications are necessary to ensure a smooth healing process.
Recovery involves several stages, beginning with immediate aftercare, continuing through long-term recovery, and includes being mindful of potential complications. Each of these stages requires specific attention and care to promote optimal healing and integration of the grafted material.
Immediate Aftercare
The first 24 to 48 hours post-surgery are crucial for setting the stage for successful recovery. During this period, patients should focus on minimizing swelling and discomfort while preventing infection.
- Apply an ice pack to the affected area to reduce swelling and discomfort.
- Take prescribed medications, including antibiotics and pain relievers, as directed.
- Avoid strenuous activities and rest as much as possible to promote healing.
- Maintain a soft diet to avoid disturbing the graft site.
- Follow strict oral hygiene practices, such as gentle rinsing with a saline solution.
It is essential to refrain from smoking and consuming alcohol during this period as they can impede the healing process and increase the risk of complications. Also, patients should avoid touching or disturbing the graft area with their tongue or fingers.
Long-Term Recovery
Long-term recovery is characterized by the integration of the graft material into the existing bone structure, which typically takes several months. The focus during this phase is to facilitate the gradual and successful incorporation of the graft while monitoring the healing process.
- Avoid chewing directly on the graft site to prevent undue stress on the healing bone.
- Maintain regular check-ups with your dentist to monitor the progress of your recovery.
- Continue following a balanced diet rich in vitamins and minerals to support bone health.
- Stay diligent with oral hygiene to prevent infection and ensure a healthy environment for the graft.
Your dentist may recommend periodic imaging tests such as X-rays to assess the integration of the graft and detect any early signs of complications.
Potential Complications
While bone grafting procedures are generally successful, being aware of potential complications can help in early detection and timely intervention. Some common complications include:
- Infection, which can be indicated by increased pain, swelling, or the presence of pus.
- Graft rejection or failure, where the graft does not integrate with the existing bone.
- Excessive bleeding that persists beyond the normal post-operative period.
- Nerve damage, which might manifest as persistent numbness or tingling in the area.
If you notice any of these symptoms, it is crucial to contact your dentist immediately to address the issue before it exacerbates. Proactive management and following post-operative instructions diligently can significantly reduce the likelihood of complications and promote a smooth recovery.
For a deeper understanding of bone grafting and related procedures, consider exploring our other articles which provide comprehensive insights into various aspects of dental implantology and regenerative techniques.
Cost and Insurance Considerations
When considering dental implants, understanding the cost and insurance considerations is essential. The costs associated with dental implants can vary widely based on several factors, and not all insurance plans cover these procedures. However, various financing options can help make this essential dental work more accessible.
In the following sub-sections, we will delve deeper into the factors affecting the cost of dental implants, the extent of insurance coverage, and available financing options to help you make an informed decision.
Factors Affecting Cost
The cost of dental implants varies significantly based on a variety of factors. One of the primary determinants is the complexity of the procedure. Simple cases with adequate bone structure will generally cost less than those requiring extensive bone grafting or sinus lifts.
Other factors that influence the cost include the materials used, the number of implants required, and the expertise of the dental professional performing the procedure. Additionally, geographical location can also play a role, with costs varying from one region to another.
Another critical factor is the type of implant and restoration chosen. For instance, mini-implants are generally less expensive than traditional implants. Moreover, the need for additional procedures such as extractions or temporary restorations can also add to the overall cost.
Insurance Coverage
Insurance coverage for dental implants can be complicated. Many dental insurance plans do not cover implants as they are often considered a cosmetic procedure. However, some plans may cover part of the cost, especially if the implant is necessary for medical reasons.
It’s essential to review your insurance policy and consult with your insurance provider to understand what is covered. Some policies may cover aspects like extractions, bone grafting, or even the crown that goes on top of the implant, even if they do not cover the implant itself.
Additionally, patients may also check if their medical insurance provides any coverage, especially in cases where the dental implant surgery is deemed medically necessary. Being well-informed can help you leverage any potential benefits.
Financing Options
Given the potentially high out-of-pocket cost of dental implants, various financing options are available to make the procedure more affordable. Many dental clinics offer payment plans that allow you to spread the cost over several months or even years.
Financing companies that specialize in medical and dental expenses can provide loans specifically designed for these types of procedures. These loans often come with flexible repayment terms and sometimes offer low or no-interest periods.
Another option to explore is credit cards specifically designed for medical and dental expenses. These cards often provide special financing offers, making them a viable option for those needing immediate dental care but unable to pay the full amount upfront. Lastly, some employers offer flexible spending accounts (FSAs) or health savings accounts (HSAs), which allow you to use pre-tax dollars for medical expenses, including dental implants. Utilizing these accounts can result in significant savings.
Understanding the cost and insurance considerations for dental implants can be complex but is crucial for making an informed decision. For more information on this topic and others related to dental health, be sure to check out our other articles.
Bone Grafting Techniques for Dental Implants
When considering dental implants, understanding the techniques and materials used in bone grafting is essential for optimal results. Here’s a brief exploration into how bone grafting works specifically for dental implants.
What role does biomaterial play in bone grafting for implants?
In bone grafting for dental implants, biomaterials act as a scaffold, facilitating the growth and integration of new bone. Autologous bone, possibly combined with a biomaterial, is used to overcorrect the implant site by 1 or 2 mm, promoting better stability and durability of the implant. The biomaterial supports the structure of the graft while it integrates with the natural bone, which is crucial during the remodeling phase when the graft may lose some height and volume.

My name is Salman Kapa, a 73-year-old expert in bone regeneration and dental implantology. With decades of experience in the field, I am dedicated to advancing our understanding of oral health and hygiene. Through my research and writing, I aim to contribute to the development of innovative solutions in dental care.