When considering a dental implant, one common issue patients face is insufficient bone density or volume, which is crucial for the stability of the implant. This scenario can arise due to various reasons, including osteoporosis, periodontal disease, or long-term tooth loss. However, advances in dental technology now offer multiple solutions to overcome this challenge. Techniques such as bone grafting and sinus lifts can provide the necessary bone structure for a successful implant. This article explores various expert approaches and innovative techniques designed to assist those lacking adequate bone support for dental implants.
Solutions for Dental Implants with Insufficient Bone
For patients who lack adequate bone to support dental implants, several innovative techniques are available to ensure successful implantation. Addressing insufficient bone is crucial as it directly impacts the long-term stability and functionality of the implants. Modern dentistry offers a range of solutions tailored to the unique needs of each patient.
Understanding the different methods to overcome bone deficiencies can help both clinicians and patients make informed decisions. This article delves into three primary techniques: bone grafting, ridge expansion, and sinus lift procedures. Each of these methods has its own set of benefits and is selected based on the specific clinical scenario.
By utilizing advanced techniques, the success rate of dental implants in patients with insufficient bone can be significantly improved. Let’s explore these techniques in more detail.
Bone Grafting Techniques
Bone grafting is a widely accepted procedure to enhance the volume and density of the bone. This technique involves the transplantation of bone tissue to the deficient area. There are several types of bone grafts:
- Autografts: Bone taken from the patient’s own body, often from the hip or another area of the jaw.
- Allografts: Bone sourced from a donor, usually through a bone bank.
- Xenografts: Bone derived from animals, typically bovine.
- Alloplasts: Synthetic or inorganic materials that mimic bone structure.
Each type of bone graft has its own advantages. Autografts have a high compatibility rate and low rejection risk since they use the patient’s own tissue. Allografts and xenografts, however, are readily available and do not require additional surgery for bone harvesting. Recent advancements in biomaterials have enhanced the effectiveness of alloplasts, making them a viable option for many patients.
Successful bone grafting can significantly improve the bone structure, providing a solid foundation for dental implants. Post-operative care and monitoring are vital to ensure the graft integrates well with the existing bone.
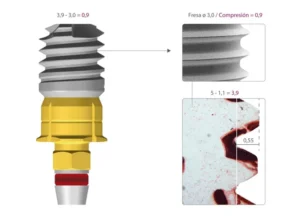
Ridge Expansion
Ridge expansion, also known as ridge splitting, is a technique used when the jawbone is not wide enough to support implants. In this procedure, the bone is surgically divided and then expanded to create a more suitable width. This method can be particularly useful in cases where bone grafting alone may not suffice.
The ridge expansion procedure is typically performed in two stages. Initially, the bone is split and allowed to heal partially. Once adequate stability is achieved, dental implants are placed. The process leverages the body’s natural healing mechanisms to create a more robust and wider bone structure.
This technique offers several advantages:
- Minimally invasive compared to extensive bone grafting.
- Reduces the overall treatment time.
- Promotes natural bone regeneration.
However, ridge expansion requires precise surgical skill and is most effective in patients with moderate bone deficiencies. It’s a suitable alternative when bone grafting is either not viable or would require excessively long healing periods.
Sinus Lift Procedures
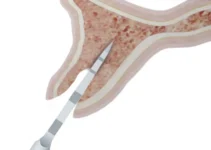
For implants in the upper jaw, especially in the area of the molars and premolars, a sinus lift procedure may be necessary. This technique is utilized when there is inadequate bone height in the upper jaw or the sinuses are too close to the jaw for implants to be placed effectively.
During a sinus lift, the sinus membrane is gently lifted, and bone is added between the jaw and the maxillary sinuses. The added bone can be from an autograft, allograft, xenograft, or alloplast. The goal is to increase bone height to support stable implant placement.
There are two main types of sinus lift procedures:
- Lateral Window Technique: An incision is made on the side of the gum to access the sinus membrane.
- Osteotome Technique: A less invasive approach where the sinus is accessed through the implant site.
The choice of technique depends on the extent of bone deficiency and the surgeon’s expertise. Sinus lifts have shown a high success rate, enabling many patients with upper jaw bone loss to receive dental implants successfully.
By understanding these techniques, patients can better appreciate the range of solutions available to overcome insufficient bone, leading to successful dental implant outcomes. For more detailed explorations of other dental health topics, be sure to read our other articles.
Expert Opinions on Dental Implant Challenges
Dental implants have revolutionized the field of dentistry by providing a reliable and long-lasting solution for missing teeth. However, despite their high success rates, implants carry certain challenges and complications that clinicians must navigate. Gaining insights from expert opinions can significantly help in understanding and addressing these challenges effectively.
Technological advancements and continuous research play pivotal roles in improving the success rates of dental implants. Yet, even the most experienced practitioners face obstacles that require meticulous planning and precision. Let’s delve into what experts say about common complications and the best practices to mitigate these issues.
Common Complications
While dental implants boast a success rate of approximately 95%, complications do arise. Peri-implantitis is one of the most frequently encountered issues. It is an inflammatory condition affecting the soft and hard tissues surrounding the implant, potentially leading to implant failure if not addressed promptly. Factors contributing to this condition include poor oral hygiene, smoking, and systemic diseases like diabetes.
Another common complication is implant rejection or failure to osseointegrate. Osseointegration is the process where the implant fuses with the jawbone. Failure of this process can occur due to poor bone quality, infection, or excessive load on the implant during the healing period. Experts suggest close monitoring and regular follow-ups to detect early signs of complications.
Nerve damage is another risk, particularly in the lower jaw where the alveolar nerve runs. Improper placement of the implant can lead to transient or, in severe cases, permanent numbness. Advanced imaging techniques, like CBCT (Cone Beam Computed Tomography), are recommended to minimize this risk.
Best Practices
To mitigate these complications, experts recommend a series of best practices. Pre-operative planning is crucial. Thorough patient assessment, including medical history and imaging studies, can help in identifying potential risk factors. Customized treatment plans tailored to individual patient needs generally yield better outcomes.
Aseptic techniques during surgical procedures are paramount to avoid infections. These include sterilization of instruments, proper surgical attire, and the use of antibiotic prophylaxis when necessary. Additionally, the surgical skill and experience of the clinician significantly influence implant success.
Post-operative care is equally important. Patients should be educated on maintaining excellent oral hygiene to prevent peri-implantitis. Regular follow-up visits enable early detection and management of any complications. For patients with systemic conditions like diabetes, managing these diseases effectively can improve implant prognosis.
In conclusion, understanding common complications and adhering to best practices can greatly enhance the success rates of dental implants. Continuous education and staying updated with the latest advancements are essential for any dental professional involved in implantology.
Explore our other articles to deepen your understanding of various aspects of dental care and advancements in implantology.
Post-Procedure Care for Dental Implants
Dental implants are an excellent solution for replacing missing teeth, offering a long-term and durable option when compared to traditional dentures or bridges. However, the success of a dental implant greatly depends on how well you care for it after the procedure. Proper post-procedure care can ensure the longevity and functionality of your dental implants. In this article, we will discuss immediate post-op care, long-term maintenance, and signs of potential problems related to dental implants.
Immediate Post-Op Care
Immediately after your dental implant procedure, it is crucial to follow specific guidelines to promote healing and minimize the risk of complications. The first 24 to 48 hours are particularly important. During this period, avoid disturbing the surgical site, refrain from vigorous rinsing, spitting, or touching the implant area. These actions can disrupt the healing process and increase the risk of infection.
For pain management, your dentist will likely prescribe pain medication or advise over-the-counter options. Applying an ice pack to the affected area can also help reduce swelling and discomfort. Stick to a soft diet for the first few days, avoiding foods that are too hot, spicy, or hard. This not only reduces strain on the implants but also prevents irritation to the gums.
Oral hygiene is vital during the healing process. You may be advised to use a special mouthwash to keep the area clean without causing irritation. Gentle brushing around the implant site is recommended, but be cautious and avoid direct contact with the implant area in the initial days.
Long-Term Maintenance
Once the initial healing period has passed, long-term care becomes the focus. Maintaining excellent oral hygiene is essential for the longevity of your dental implants. Brush your teeth at least twice a day using a soft-bristle toothbrush and non-abrasive toothpaste. Floss daily to remove plaque and food particles from between your teeth and around the implant. Regular dental check-ups are a must. Your dentist will monitor the condition of your implants and the surrounding gum tissue, ensuring that everything is healing properly and detecting any potential issues early on. Professional cleanings are also recommended to maintain optimal oral health.
Avoid habits that can damage your implants, such as smoking, which can impair healing and increase the risk of implant failure. Refrain from chewing on hard items like ice or nutshells, as this can cause mechanical damage to the implant and surrounding teeth.
Signs of Potential Problems
While dental implants have a high success rate, it is essential to be aware of signs that may indicate problems. Early detection and intervention can prevent minor issues from becoming major complications. Look out for persistent pain, which could indicate infection or other underlying issues. If you experience severe discomfort that doesn’t improve with medication, contact your dentist immediately.
Swelling or redness around the implant site beyond the initial healing period can be a sign of infection or inflammation. Any unusual changes in the implant’s stability, such as feeling loose or shifting, should be reported to your dentist right away.
Other signs to watch for include difficulty chewing, a strange taste in your mouth, or signs of gum disease around the implant. Regular self-examinations and professional check-ups can help you stay ahead of any potential problems. By following these guidelines for post-procedure care, you can maximize the success and longevity of your dental implants. For more information on maintaining optimal oral health and understanding other dental treatments, explore our other articles.
Common Questions About Dental Implants With Insufficient Bone
When considering dental implants, the amount of available bone is a critical factor. Here are some frequently asked questions for those concerned about bone deficiency and implant options.
What are the options if I have insufficient bone for dental implants?
If your dental evaluation shows insufficient bone density or volume for implants, several techniques can be employed to improve the situation. Bone grafting is the most common solution, where bone from another source is used to enhance the deficient area. Other techniques include sinus lifts for upper jaw implants and ridge expansion to widen the bone structure. Each technique aims to create a suitable environment for implant placement.
How successful are dental implants after bone regeneration procedures?
Dental implants following bone regeneration procedures generally show a high success rate, similar to standard implants. The key to success involves proper surgical technique, adequate healing time, and continuous follow-up care. Patients who undergo bone augmentation need to maintain excellent oral hygiene and follow their dentist’s instructions closely to ensure the best outcomes.

My name is Salman Kapa, a 73-year-old expert in bone regeneration and dental implantology. With decades of experience in the field, I am dedicated to advancing our understanding of oral health and hygiene. Through my research and writing, I aim to contribute to the development of innovative solutions in dental care.