Understanding your ovarian reserve through medical testing is crucial for assessing fertility potential. Several key tests, including Anti-Müllerian Hormone (AMH), Follicle Stimulating Hormone (FSH), and antral follicle count via ultrasound, provide valuable insights into a woman’s reproductive capacity. These tests measure different aspects of ovarian function, helping doctors evaluate egg quantity and quality. While interpreting results requires medical expertise, knowing your numbers can help you make informed decisions about family planning and fertility treatments.
Understanding Ovarian Reserve
The concept of ovarian reserve represents a crucial aspect of female reproductive health, serving as a key indicator of a woman’s reproductive potential. Ovarian reserve refers to both the quantity and quality of eggs remaining in a woman’s ovaries at any given time, which naturally declines with age. Research has consistently shown that fertility begins to decline significantly in most women starting in their mid-30s, with a more dramatic decrease after age 37. This biological reality makes understanding ovarian reserve particularly important for women planning their reproductive future.
Modern reproductive medicine has developed various testing methods to assess ovarian reserve, providing valuable insights into a woman’s reproductive potential and helping guide treatment decisions for those experiencing fertility challenges.
What is Ovarian Reserve?
Ovarian reserve specifically describes the functional potential of the ovaries to produce eggs that are capable of fertilization resulting in healthy pregnancies. Women are born with approximately 1-2 million immature eggs, and this number progressively decreases throughout their reproductive lives.
The decline in ovarian reserve involves both quantitative and qualitative changes. As women age, they experience a reduction in both the number of remaining eggs and their genetic quality. This natural process is influenced by various factors including:
- Genetic predisposition
- Environmental factors
- Medical conditions affecting the ovaries
- Previous ovarian surgery
- Exposure to certain medications or treatments
Understanding these factors helps healthcare providers better evaluate and manage fertility potential in their patients.
Why Test Ovarian Reserve?
Ovarian reserve testing serves as a valuable tool for both patients and healthcare providers in assessing reproductive potential and planning appropriate fertility treatments. These tests can help predict how well a woman might respond to fertility medications and estimate her remaining reproductive window.
Testing is particularly recommended for women who:
- Are over 35 and trying to conceive
- Have a family history of early menopause
- Have had previous ovarian surgery
- Have experienced chemotherapy or radiation therapy
- Have unexplained infertility
Early testing can provide crucial information for family planning decisions and help identify potential fertility issues before they become critical. The results can guide treatment strategies and timing, potentially improving the chances of successful conception.
Understanding your ovarian reserve is just one aspect of fertility assessment. We encourage you to explore our other articles about fertility testing, treatment options, and reproductive health to gain a comprehensive understanding of your reproductive journey.
Main Ovarian Reserve Tests
Evaluating ovarian reserve is a crucial first step in fertility assessment. Modern reproductive medicine relies on several validated tests that provide valuable insights into a woman’s reproductive potential. These tests help clinicians assess the quantity and quality of remaining eggs, enabling more accurate fertility planning and treatment recommendations.
The most reliable and widely used ovarian reserve tests include blood hormone measurements and ultrasound imaging. Each test offers unique advantages and, when used in combination, provides a comprehensive picture of reproductive health. Understanding these tests is essential for both healthcare providers and patients to make informed decisions about fertility treatments.
Anti-Müllerian Hormone (AMH) Test
The AMH test has emerged as the gold standard for ovarian reserve testing. This hormone is produced by small follicles in the ovaries and provides a reliable indicator of the remaining egg supply. Unlike other hormone tests, AMH levels remain relatively stable throughout the menstrual cycle, making it possible to perform the test at any time.
Test results are measured in nanograms per milliliter (ng/mL), with typical ranges varying by age. Generally, higher AMH levels indicate a larger ovarian reserve:
- Optimal fertility: > 1.0 ng/mL
- Low reserve: 0.5-1.0 ng/mL
- Very low reserve: < 0.5 ng/mL
Regular monitoring of AMH levels can help track changes in ovarian reserve over time, allowing for better-informed family planning decisions and fertility treatment strategies.
Follicle Stimulating Hormone (FSH) Test
FSH testing is traditionally performed on day 3 of the menstrual cycle to assess ovarian function. This hormone, produced by the pituitary gland, stimulates follicle development in the ovaries. When ovarian function declines, FSH levels typically increase as the body attempts to compensate.
Interpretation of FSH results requires consideration of other hormones, particularly estradiol. Normal FSH levels on day 3 typically fall between 4-13 IU/L, with levels above 10 IU/L potentially indicating reduced ovarian reserve.
Monthly variations can occur, making it important to consider multiple FSH measurements over time for the most accurate assessment. Higher FSH levels may indicate diminished ovarian reserve or the approach of menopause.
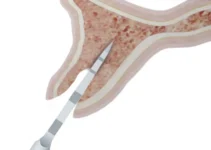
Antral Follicle Count (AFC)
AFC involves a transvaginal ultrasound examination to count the number of small antral follicles present in both ovaries. This test is typically performed during the early follicular phase of the menstrual cycle, usually between days 2-5.
During the procedure, the technician counts follicles measuring 2-10 millimeters in diameter. The total number provides a good indication of ovarian reserve:
- High: > 20 follicles
- Normal: 8-20 follicles
- Low: < 8 follicles
AFC results strongly correlate with both AMH levels and response to fertility treatments. This visual assessment provides immediate results and can help predict how well a woman might respond to fertility medications.
Understanding your ovarian reserve is crucial for making informed decisions about fertility. For more detailed information about specific fertility treatments and success rates, we encourage you to explore our related articles on fertility preservation options and advanced reproductive technologies.
Interpreting Test Results
Understanding ovarian reserve test results is crucial for making informed decisions about fertility treatment. The interpretation requires considering multiple factors including age-specific reference ranges and individual circumstances. These tests provide valuable insights into a woman’s reproductive potential and help doctors recommend the most appropriate treatment options. The most reliable approach is to analyze results from multiple tests together, as no single test can perfectly predict fertility outcomes. AMH levels, antral follicle count (AFC), and FSH levels are typically evaluated in combination to provide a comprehensive assessment of ovarian reserve.
Normal Range Values
Normal ovarian reserve test results generally fall within these ranges for women of reproductive age:
- AMH levels: 1.0-4.0 ng/mL
- AFC: 8-15 follicles total (both ovaries combined)
- Day 3 FSH: 4.7-8.6 mIU/mL
- Estradiol: 20-80 pg/mL
These ranges indicate healthy ovarian function and suggest a good probability of response to fertility treatments. However, it’s important to note that normal values can vary slightly between laboratories and age groups.
Low Ovarian Reserve Indicators
Several test results may indicate diminished ovarian reserve (DOR):
- AMH levels below 1.0 ng/mL
- AFC of less than 5-7 follicles
- FSH levels above 10 mIU/mL
- Elevated estradiol levels on day 3
These results suggest reduced fertility potential and may indicate a need for more aggressive treatment approaches. However, women with low ovarian reserve can still achieve pregnancy, especially with appropriate medical intervention and timing.
It’s crucial to understand that low ovarian reserve doesn’t necessarily mean infertility, but rather indicates a potentially shorter reproductive window and may affect treatment success rates.
High Ovarian Reserve Indicators
High ovarian reserve values typically include:
- AMH levels above 4.0 ng/mL
- AFC greater than 15-20 follicles
- Very low FSH levels (below 4.0 mIU/mL)
While high ovarian reserve might seem advantageous, it can sometimes indicate conditions like polycystic ovary syndrome (PCOS). These patients may require careful monitoring during fertility treatments to prevent ovarian hyperstimulation syndrome.
Women with high ovarian reserve generally have good fertility potential but may need specialized treatment protocols to optimize outcomes and minimize risks.
For more detailed information about specific fertility treatments and their success rates, we encourage you to explore our related articles on fertility preservation options and advanced reproductive technologies.
Next Steps After Testing
Understanding your ovarian reserve test results is crucial for making informed decisions about your fertility journey. Test results typically fall into three categories: normal range, borderline, or indicating diminished ovarian reserve. Each category requires a different approach and treatment strategy.
The interpretation of these results should always be done in conjunction with other factors such as age, overall health, and fertility goals. Time is a critical factor in fertility treatment decisions, particularly for women with diminished ovarian reserve or advanced maternal age.
Medical professionals typically recommend creating a personalized fertility plan based on test results, which may include immediate intervention or a more gradual approach depending on individual circumstances.
Treatment Options
Different test results may indicate various treatment paths. For patients with normal ovarian reserve, options might include:
- Natural conception with timed intercourse
- Intrauterine insemination (IUI)
- In vitro fertilization (IVF)
- Fertility medication protocols
For those with diminished ovarian reserve, more aggressive treatment approaches might be recommended, such as immediate IVF treatment or consideration of egg donation programs. The success rates vary significantly depending on individual circumstances and chosen treatment methods.
Recent advances in reproductive technology have expanded the available options, including procedures like preimplantation genetic testing and various ovarian stimulation protocols tailored to specific patient needs.
Lifestyle Modifications
Regardless of test results, certain lifestyle changes can positively impact fertility potential. Key modifications include:
- Maintaining a healthy BMI
- Following a fertility-friendly diet rich in antioxidants
- Regular moderate exercise
- Stress reduction techniques
- Avoiding tobacco and limiting alcohol consumption
Research shows that implementing these lifestyle changes can improve overall reproductive health and potentially enhance the success rates of fertility treatments. Timing is crucial, and these modifications should be implemented as soon as possible.
When to Seek Additional Testing
Additional fertility testing might be necessary in several scenarios. Key indicators for further testing include:
- Unexpected poor response to initial fertility treatments
- Significant changes in menstrual cycles
- Age-related concerns
- Family history of early menopause
Regular monitoring and reassessment of ovarian reserve may be recommended, particularly for women with borderline results or those undergoing fertility treatments. Early detection of changes can allow for timely adjustment of treatment strategies.
Understanding your fertility status is an ongoing process. For more detailed information about specific treatment options or to learn about the latest advances in fertility care, we encourage you to explore our other comprehensive guides on reproductive health and fertility preservation techniques.
Understanding Ovarian Reserve Testing and Results
Ovarian reserve testing is crucial for assessing fertility potential. Understanding these tests and their results can help patients make informed decisions about their reproductive journey.
What do ovarian reserve test results tell us about fertility potential?
Ovarian reserve test results provide valuable information about the quantity and quality of remaining eggs. The main indicators include FSH (Follicle Stimulating Hormone), AMH (Anti-Müllerian Hormone), and antral follicle count via ultrasound. Normal AMH levels typically range from 1.0-4.0 ng/mL, with higher values indicating better ovarian reserve. FSH levels under 10 mIU/mL are considered optimal. These results help doctors assess fertility potential and guide treatment options, though they don’t definitively predict pregnancy success.