Apneic episodes, often associated with sleep apnea, are characterized by brief interruptions in breathing during sleep. These disruptions can significantly impact the quality of sleep and overall health, leading to daytime fatigue, cardiovascular issues, and other serious health conditions. Understanding the causes, symptoms, and potential treatment options for apneic episodes is crucial for those affected. This article delves into the mechanisms behind these episodes and explores effective strategies to manage and reduce their occurrences, thereby improving sleep quality and health outcomes.
What Are Apneic Episodes?
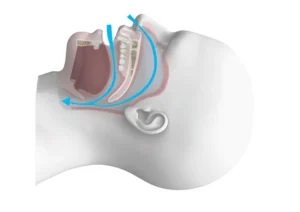
Apneic episodes refer to moments when a patient experiences a temporary cessation of breathing, typically during sleep. These episodes can last anywhere from a few seconds to minutes and often occur multiple times throughout the night. The most common type is Obstructive Sleep Apnea (OSA), which involves repetitive episodes of partial or complete blockage of the upper airway during sleep. This leads to reduced blood oxygen saturation and fragmented sleep.
The primary causes of apneic episodes include anatomical factors, such as the size and shape of the airway, as well as functional issues like the relaxation of muscles in the throat. Other contributing factors include obesity, which can increase the likelihood of airway obstruction, and certain lifestyle choices such as smoking and alcohol consumption. Moreover, central sleep apnea occurs when the brain fails to send the appropriate signals to the muscles that control breathing.
- Obstructive Sleep Apnea (OSA)
- Central Sleep Apnea (CSA)
- Complex Sleep Apnea Syndrome
Understanding the implications of apneic episodes is crucial for effective diagnosis and treatment. These episodes not only disrupt sleep but can also have significant long-term health consequences, including cardiovascular diseases, hypertension, diabetes, and cognitive impairments. For those experiencing any symptoms of sleep apnea, such as loud snoring, choking or gasping during sleep, daytime fatigue, and difficulty concentrating, consulting a healthcare provider for a comprehensive evaluation is essential.
For more in-depth information on related topics, consider reading our other articles on sleep disorders, their diagnosis, and advanced treatment options.
Causes and Risk Factors of Apneic Episodes
Sleep apnea is a potentially serious sleep disorder where breathing repeatedly stops and starts. These interruptions, known as apneic episodes, can be caused by various factors, which are generally categorized into three primary types: obstructive, central, and complex sleep apnea. Understanding the causes and risk factors for each type is crucial for effective diagnosis and treatment.
Factors such as age, weight, and lifestyle choices can significantly influence the likelihood of developing sleep apnea. It’s essential to recognize the specific elements that contribute to each type of apnea to tailor appropriate interventions and management strategies. In the following sections, we will explore the causes and risk factors of obstructive, central, and complex sleep apnea in detail.
While these conditions share some commonalities, each has unique triggers and associated risks. By identifying these distinct factors, we can better understand and address the complexities of sleep apnea, enhancing patient outcomes and promoting healthier sleep patterns.
Obstructive Sleep Apnea
Obstructive Sleep Apnea (OSA) occurs when the muscles at the back of the throat fail to keep the airway open, despite efforts to breathe. The most common cause is the relaxation of these muscles during sleep, leading to a blockage of airflow. Some prevalent causes include:
- Excess weight, as fatty deposits around the upper airway can obstruct breathing.
- Neck circumference, as individuals with thicker necks may have narrower airways.
- A narrowed airway, either genetically or due to enlarged tonsils or adenoids.
The risk factors for OSA also include gender (more common in men), age (risk increases with age), and family history. Lifestyle factors such as smoking, alcohol use, and sedentary habits can further exacerbate the condition. Continuous monitoring and lifestyle modifications are crucial for managing OSA effectively.
Central Sleep Apnea
Central Sleep Apnea (CSA) is less common than OSA and involves the brain’s failure to send proper signals to the muscles that control breathing. This type is often linked to serious illnesses and conditions affecting the brainstem, which controls breathing. The primary causes include:
- Heart disorders, such as congestive heart failure.
- Stroke or other neurological conditions.
- High-altitude periodic breathing due to low oxygen levels at high altitudes.
Risk factors for CSA include being male and increasing age. Use of narcotic pain medications or other drugs that affect the brain can also contribute to the development of CSA. Unlike OSA, CSA requires specialized treatments that often focus on the underlying health issues contributing to the condition.
Complex Sleep Apnea Syndrome
Complex Sleep Apnea Syndrome, also known as treatment-emergent central sleep apnea, combines elements of both obstructive and central sleep apnea. It typically emerges when a patient being treated for OSA with Continuous Positive Airway Pressure (CPAP) develops central apneic episodes. The causes are not entirely understood, but it is believed to be a combination of anatomical and neurological factors.
Risk factors for complex sleep apnea syndrome include those for OSA, such as obesity and male gender, as well as factors contributing to CSA. Additionally, the use of CPAP therapy can sometimes unmask central apneas in patients with a predisposition to central apnea.
Effective management of this syndrome requires a nuanced approach, often combining therapies used for both OSA and CSA. Understanding the underlying causes and individualized treatment plans are essential for addressing this multifaceted condition.
Recognizing and understanding the causes and risk factors of different types of sleep apnea is essential for accurate diagnosis and effective management. By doing so, we can improve the quality of life for those affected by this potentially debilitating condition. For more insights on sleep disorders and their implications, be sure to check out other articles on our website.
Health Implications of Apneic Episodes
Apneic episodes, or temporary cessations of breathing during sleep, pose significant health risks that many individuals might not be fully aware of. These episodes can contribute to a variety of serious health complications that, if left untreated, may affect one’s overall quality of life. Understanding these implications is crucial for both patients and healthcare providers in order to manage and mitigate the risks associated with sleep apnea.
One of the most concerning consequences of apneic episodes is their impact on the cardiovascular system. Repeated interruptions in breathing can lead to fluctuations in blood oxygen levels, which place undue stress on the heart and blood vessels. Additionally, the resultant sleep fragmentation from these episodes contributes to chronic fatigue, which in turn can affect cognitive function and mood. Clearly, the health implications of apneic episodes extend far beyond disrupted sleep.
In this section, we will delve into the specific health effects of apneic episodes, focusing on their cardiovascular effects and the resultant daytime fatigue and cognitive impairment that sufferers often experience. By gaining a comprehensive understanding of these issues, individuals can seek appropriate treatments and lifestyle changes to improve their health outcomes.
Cardiovascular Effects
The cardiovascular system is particularly vulnerable to the effects of apneic episodes. Frequent pauses in breathing lead to decreased oxygen levels in the blood, which can cause fluctuations in blood pressure. These fluctuations can strain the heart, making it work harder to pump blood effectively. Over time, this added strain can contribute to the development of hypertension, also known as high blood pressure, which is a significant risk factor for heart disease and stroke. Studies have shown that individuals with untreated sleep apnea are at a higher risk of suffering from various cardiovascular problems. These include arrhythmias, or irregular heartbeats, which can disrupt the normal rhythm of the heart and potentially lead to more serious conditions such as atrial fibrillation. In severe cases, the repeated stress on the cardiovascular system can even result in heart failure.
The link between sleep apnea and cardiovascular health is well-documented. For instance, research published in the *Journal of the American College of Cardiology* highlights that treating sleep apnea can significantly reduce blood pressure and improve overall heart function. This emphasizes the importance of identifying and managing sleep apnea to protect cardiovascular health.
Daytime Fatigue and Cognitive Impairment
Another significant consequence of apneic episodes is daytime fatigue. The repeated interruptions in breathing cause frequent awakenings or arousals during the night, preventing sufferers from achieving restful and restorative sleep. As a result, individuals with sleep apnea often experience excessive daytime sleepiness, which can severely impact their daily lives. This chronic fatigue can reduce productivity, increase the risk of accidents, and negatively affect one’s overall well-being.
Aside from physical tiredness, sleep apnea can also lead to cognitive impairment. Poor sleep quality affects the brain’s ability to process and retain information, resulting in difficulties with memory, concentration, and decision-making. This cognitive decline can be particularly concerning for those whose jobs require high levels of mental acuity, such as professionals working in fields that demand precision and attention to detail.
Research has shown that untreated sleep apnea can also heighten the risk of developing more serious cognitive disorders, including dementia. A study published in *Neurology* found that older adults with sleep apnea are more likely to experience a decline in cognitive function. Therefore, addressing sleep apnea not only helps alleviate daytime fatigue but also preserves cognitive health.
In conclusion, the health implications of apneic episodes are multifaceted and far-reaching. From cardiovascular risks to cognitive challenges, the impact of these interruptions in breathing during sleep should not be underestimated. By recognizing and treating sleep apnea, individuals can significantly enhance both their physical and mental health, leading to a better quality of life. Additionally, readers interested in learning more about related health topics can explore our other articles for further information and insights.
Common Concerns About Apneic Episodes
Understanding apneic episodes is crucial for recognizing the effects of sleep apnea on health. Here’s a frequently asked question about this condition.
What are apneic episodes and how do they affect sleep quality?
Apneic episodes are periods during sleep when breathing stops or becomes significantly shallow, typically due to a blockage in the airway or a failure in respiratory signaling. These interruptions can last from a few seconds to over a minute and often lead to a sudden awakening. As a result, sleep quality suffers, causing increased day-time sleepiness, impaired cognitive function, and higher risks of cardiovascular issues.

My name is Salman Kapa, a 73-year-old expert in bone regeneration and dental implantology. With decades of experience in the field, I am dedicated to advancing our understanding of oral health and hygiene. Through my research and writing, I aim to contribute to the development of innovative solutions in dental care.