Dental bone regeneration is a pivotal process in ensuring the stability and longevity of dental implants. This technique involves various strategies to restore bone loss in the jaw, which often occurs due to periodontal disease, injury or atrophy following tooth loss. It lays the foundation for successful implant integration by providing the necessary bone density and volume. Understanding the key procedures like bone grafting and guided tissue regeneration can greatly influence post-operative outcomes and overall dental health.
Types of Dental Bone Regeneration Techniques
Dental bone regeneration is a crucial aspect of modern implantology, ensuring that patients have sufficient bone density for the successful placement of dental implants. Several techniques have been developed to address different patient needs and conditions. In this section, we will explore the most commonly used methods, each with its inherent benefits and limitations.
The main goal of bone regeneration techniques is to promote the body’s natural ability to regenerate bone tissue, providing a stable and robust foundation for dental implants. By understanding the different types and their applications, clinicians can make informed decisions to achieve the best outcomes for their patients.
Guided Bone Regeneration (GBR)
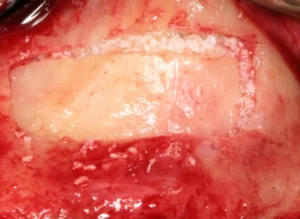
Guided Bone Regeneration (GBR) is a widely-used technique that involves using barrier membranes to direct the growth of new bone tissues at the desired sites. This method helps in preventing soft tissues from invading the new bone growth area, allowing for optimal bone regeneration. GBR is particularly effective in cases where there is minor to moderate bone loss.
One of the main advantages of GBR is its ability to use resorbable or non-resorbable membranes. Resorbable membranes dissolve over time, eliminating the need for a second surgery to remove them. Non-resorbable membranes, on the other hand, offer superior structural support but require additional surgical intervention for removal.
Studies have shown that GBR can significantly improve the success rate of dental implants by creating a stable bone foundation. Key factors that influence the success of GBR include the choice of membrane material, the patient’s health condition, and the precision of the surgical technique.
Autogenous Bone Grafts
Autogenous bone grafts, also known as autografts, involve harvesting bone tissue from the patient’s own body, often from areas such as the chin, jaw, hip, or tibia. This technique is considered the gold standard in bone regeneration due to its high biocompatibility and osteogenic potential. Autografts contain live bone cells that promote natural bone healing and growth. One of the significant advantages of using autogenous bone grafts is the reduced risk of immune rejection since the bone is sourced from the same individual. However, this technique requires an additional surgical site, which can increase the complexity and recovery time of the procedure.
Clinical studies have demonstrated that autogenous bone grafts achieve excellent results in both horizontal and vertical bone augmentations. The success of this method largely depends on the skill of the surgeon and the quality of the harvested bone tissue.
Allogenic Bone Grafts
Allogenic bone grafts, or allografts, use bone tissue sourced from a donor of the same species, typically obtained from bone banks. These grafts undergo rigorous processing and sterilization to ensure they are safe for transplantation. Allografts are often used when large volumes of bone are needed, and harvesting autogenous bone would be impractical or undesirable.
One of the primary benefits of allogenic bone grafts is that they eliminate the need for a second surgical site, thereby reducing the overall surgical risk and patient discomfort. However, because the bone comes from a different individual, there is a slight risk of immune reaction or disease transmission, although this is minimized by thorough screening and processing.
Allografts are available in different forms, including freeze-dried bone and demineralized bone matrix, each with unique properties that can affect the outcome of the regeneration process. Studies have shown that while allografts may not be as osteogenic as autografts, they are highly effective in providing structural support and serving as a scaffold for new bone growth.
Understanding the various dental bone regeneration techniques allows clinicians to tailor treatments to individual patient needs, optimizing outcomes and enhancing the longevity of dental implants. To dive deeper into each of these methods and explore other advanced techniques in implantology, be sure to check out our other articles on the latest advancements in dental procedures.
Factors Influencing the Success of Dental Bone Regeneration
Dental bone regeneration is a critical aspect of modern implantology, allowing patients with insufficient bone mass to receive dental implants. The success of bone regeneration largely depends on a combination of factors, including the patient’s health, the quality of the bone graft material, and the surgical techniques employed. Understanding these factors can significantly impact the outcomes of the procedure.
Several clinical studies have demonstrated the importance of each of these factors. From optimizing patient conditions to selecting the appropriate graft materials and utilizing advanced surgical techniques, each aspect plays a crucial role in ensuring long-term success and patient satisfaction.
Patient’s Health and Lifestyle
The overall health and lifestyle of a patient are paramount in determining the success of dental bone regeneration. Patients with certain medical conditions, such as diabetes or osteoporosis, may experience slower healing and integration of the graft material. Additionally, habits like smoking can significantly impede the healing process, leading to compromised outcomes. Maintaining a healthy lifestyle is crucial for optimal bone regeneration. Factors such as a balanced diet, regular exercise, and avoiding negative habits like smoking and excessive alcohol consumption can create a favorable environment for bone regeneration.
Preoperative assessments should include a thorough review of the patient’s medical history, including any chronic conditions or medications that may impact bone healing. This assessment allows for a more tailored approach to treatment, potentially improving the chances of success.
Quality of Bone Graft Material
The type and quality of the bone graft material are essential for the success of dental bone regeneration. Various materials are available, including autografts, allografts, xenografts, and synthetic options. Each type has its own set of advantages and limitations.
Autografts, or bone grafts taken from the patient’s own body, are often considered the gold standard due to their high compatibility and success rates. However, they also come with the drawback of requiring an additional surgical site, which can increase recovery time and patient discomfort.
- Allografts: Donor bone from a different person, typically processed to reduce risk of infection.
- Xenografts: Bone from a different species, often bovine, processed to be biocompatible.
- Synthetic materials: Manufactured materials designed to mimic natural bone properties.
Each graft material choice should be made based on the specific needs and conditions of the patient, aiming to maximize integration and stability of the new bone.
Surgical Techniques Employed
The surgical techniques used during the bone regeneration process play a significant role in the procedure’s outcome. Meticulous surgical practices can minimize trauma to the surrounding tissues and improve the integration of the graft material.
Advanced techniques such as guided bone regeneration (GBR) and the use of growth factors can enhance the success rates of bone grafts. GBR involves the use of barrier membranes to direct the growth of new bone, ensuring that the graft material remains in place during the healing process. Growth factors can stimulate cellular activities, promoting faster and more efficient bone regeneration.
Moreover, the surgeon’s experience and skill level are critical. Experienced practitioners are more adept at managing complications and ensuring that the graft is placed accurately, which can significantly impact the overall success of the procedure.
Understanding these factors and their influence on dental bone regeneration can help both practitioners and patients make informed decisions, leading to better outcomes. To dive deeper into the intricacies of dental treatments, explore our other articles that cover a range of topics in implantology and regenerative dentistry.
Impact of Dental Bone Regeneration on Implant Success
The success of dental implants is significantly influenced by the quality and quantity of the surrounding bone. Dental bone regeneration techniques have evolved to address the challenges posed by bone loss due to periodontal disease, trauma, or long-term tooth absence. Regenerative procedures aim to restore sufficient bone volume and density, leading to a higher success rate of dental implants.
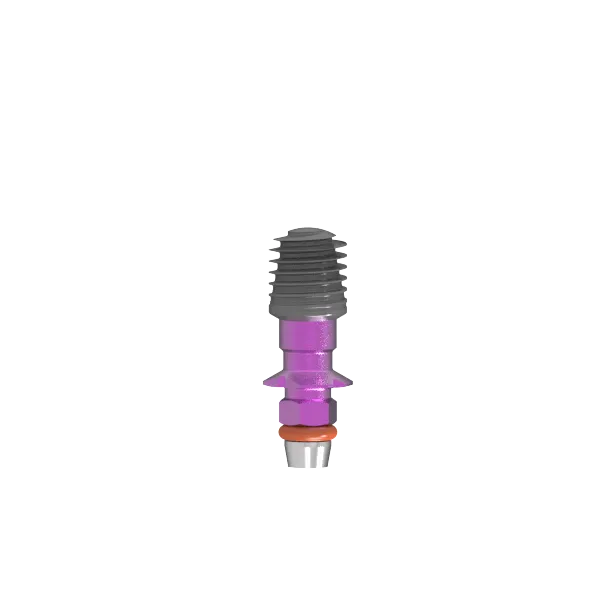
Bone regeneration is achieved through various methods, including guided bone regeneration (GBR), the use of bone grafts, and the application of growth factors. Studies have shown that these methods not only compensate for bone deficiencies but also enhance the integration of the implant with the natural bone. This integration, known as osseointegration, is crucial for the long-term stability and functionality of the implant.
Additionally, advancements in biomaterials and stem cell therapy have opened new avenues for more predictable and efficient bone regeneration. These innovative techniques contribute to the improvement of implant success rates, offering patients a reliable and durable solution for missing teeth.
Improved Implant Stability
One of the primary benefits of dental bone regeneration is the improvement in implant stability. When there is sufficient bone volume, the implant can achieve a stronger initial fixation, which is essential for the early stages of healing and osseointegration. Studies have demonstrated that patients with adequate bone support experience fewer complications and a higher rate of implant success.
Improved implant stability is closely linked to the reduction of micromovements between the implant and bone. Micromovements can hinder the osseointegration process, leading to implant failure. By ensuring optimal bone regeneration, dental professionals can minimize these movements, leading to a more stable and robust implant.
Furthermore, bone regeneration procedures often involve the use of biocompatible materials that promote bone growth around the implant. These materials, such as hydroxyapatite and tricalcium phosphate, mimic the natural bone environment, enhancing the stability and longevity of the implant.
Enhanced Aesthetic Outcomes
In addition to functional benefits, dental bone regeneration has a significant impact on the aesthetic outcomes of dental implants. Adequate bone volume ensures that the implant is placed correctly in relation to the surrounding teeth and gums, resulting in a natural-looking appearance. Aesthetics play a crucial role in patient satisfaction and overall quality of life.
Proper bone regeneration also prevents the collapse of facial structures that can occur due to bone loss. When bone volume is maintained, the contours of the face are preserved, giving patients a healthier and more youthful appearance.
Moreover, the use of advanced imaging technologies allows dentists to plan the implant placement with precision, ensuring that the prosthetic restoration aligns seamlessly with the patient’s natural dentition. This level of detail is particularly important in the esthetic zone, where even minor discrepancies can be noticeable.
By investing in dental bone regeneration procedures, patients can achieve not only lasting dental function but also enhanced visual appeal. For those interested in the broader implications of oral health and advanced dental techniques, be sure to check out our other articles on the latest trends and innovations in implantology.
Frequently Asked Questions about Dental Bone Regeneration
If you’re considering dental implants, you might have questions about the bone regeneration process essential for implant success. Here, we address some common queries to help you understand this important aspect of dental surgery.
What is dental bone regeneration and why is it important for implant procedures?
Dental bone regeneration is a procedure aimed at rebuilding or regenerating bone in the jaw where bone loss has occurred—either due to periodontal disease, trauma, or tooth extraction. This process is critical for dental implants because sufficient bone quantity and quality are necessary to support the implants, ensuring their stability and long-term success. Techniques like bone grafts, guided bone regeneration, and growth factor application are commonly employed to enhance bone density and structure before proceeding with implants.

My name is Salman Kapa, a 73-year-old expert in bone regeneration and dental implantology. With decades of experience in the field, I am dedicated to advancing our understanding of oral health and hygiene. Through my research and writing, I aim to contribute to the development of innovative solutions in dental care.