Choosing to get dental implants is a significant decision that impacts not just your oral health, but your overall quality of life. Dental implants offer a durable and aesthetically pleasing solution to missing teeth, closely mimicking the natural look and function of your original teeth. They integrate with your bone, providing stable support for artificial teeth such as crowns, bridges, or dentures. As you consider dental implants, it’s vital to understand the procedure, the required upkeep, potential risks, and the long-term benefits to ensure it’s the right choice for your dental needs.
What are Dental Implants?
Dental implants are a revolutionary advancement in modern dentistry, providing a permanent solution for those missing one or more teeth. These artificial tooth roots are placed into the jawbone, where they fuse over time, forming a stable foundation for replacement teeth. This not only restores the aesthetic appearance of a natural smile but also maintains the structural integrity of the jawbone.
Unlike dentures or bridges, dental implants offer a more durable and long-lasting alternative, greatly improving the quality of life for patients. They can help in preserving facial structure, preventing bone loss that typically occurs when teeth are missing. This article will delve into the crucial aspects of dental implants, covering their definition, types, and how they work.
Definition and Basics
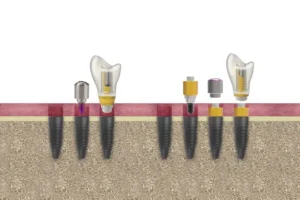
A dental implant is a titanium post that is surgically positioned into the jawbone beneath the gum line to act as a tooth root. Once in place, it allows your dentist to mount replacement teeth or a bridge into that area. Titanium is used due to its compatibility with the body, greatly reducing the risk of rejection and enhancing osseointegration, the process where the bone grows around the implant.
This process typically involves several stages:
- Initial consultation and assessment by a dental implant specialist.
- Surgical placement of the implant into the jawbone.
- A healing period, usually several months, allowing for osseointegration.
- Placement of an abutment to which the prosthetic tooth will be attached.
- Finally, placement of the prosthetic tooth, crown, or bridge.
 This step-by-step approach ensures that the implant is securely anchored and capable of supporting the replacement tooth or teeth.
This step-by-step approach ensures that the implant is securely anchored and capable of supporting the replacement tooth or teeth.
Types of Dental Implants
There are several types of dental implants available, each suited for different needs and circumstances. The main types include:
Endosteal Implants: These are the most common type of dental implants and are placed directly into the jawbone. They usually resemble small screws and are made of titanium. Once the surrounding gum tissue has healed, a second surgery is necessary to attach a post to the original implant. Finally, an artificial tooth (or teeth) is attached to the post.
Subperiosteal Implants: These implants consist of a metal frame that is fitted onto the jawbone just below the gum tissue. As the gums heal, the frame becomes fixed to the jawbone. Posts attached to the frame protrude through the gums, and artificial teeth are then mounted to these posts. This type is used primarily for patients who cannot wear conventional dentures and who have minimal bone height.
Zygomatic Implants: These are the least common and the most complex type of dental implants. They are placed in the patient’s cheekbone rather than the jawbone. Zygomatic implants are typically used when there is insufficient bone in the upper jaw, making other types of implants impossible without lengthy bone graft procedures.
How Dental Implants Work
Dental implants function by mimicking the natural roots of teeth. When a tooth is lost, the jawbone in the empty space deteriorates over time due to the lack of stimulation from chewing. Implants help prevent this bone loss by providing the necessary stimulation to the jawbone.
The success of dental implants relies heavily on osseointegration, where the bone cells grow around the titanium post. This fusion process ensures a stable bond, allowing the implant to function like a natural tooth root. Factors that can affect the success of osseointegration include the patient’s bone quality, oral hygiene, and overall health.
Once osseointegration is complete, the abutment is attached to the implant. The abutment acts as a connector between the implant and the prosthetic tooth. The final step is the placement of the prosthetic tooth, which is custom-made to match the size, shape, and color of the patient’s natural teeth, ensuring a seamless and natural appearance.
Understanding the entire process of how dental implants work can help patients make informed decisions about their oral health and treatment options. If you’re interested in learning more about dental implants and other dental innovations, be sure to check out our other articles.
The Implant Procedure
Dental implants have revolutionized the field of restorative dentistry by offering a long-lasting and aesthetically pleasing solution for missing teeth. The implant procedure involves several meticulous steps to ensure the successful placement and integration of the implant with the jawbone. This multi-stage process can take several months to complete, but the results are often well worth the wait. This section will guide you through the key stages of the implant procedure, from the initial consultation to the recovery phase.
Understanding the various stages of the dental implant procedure can help alleviate some of the anxiety and uncertainty associated with it. Each stage is crucial for the eventual success of the implant and involves careful planning and execution. Below, we delve into the specific steps involved in the procedure, providing you with a comprehensive understanding of what to expect.
Initial Consultation and Assessment
The initial consultation is the foundation of a successful implant procedure. During this visit, a comprehensive assessment is conducted to evaluate your oral health and determine if you are a suitable candidate for dental implants. This assessment typically includes a thorough examination of your teeth and gums, along with imaging tests such as X-rays or 3D scans. These imaging tests provide detailed information about the density and structure of your jawbone, which is crucial for planning the implant placement.
In addition to the physical examination, your dental history and general health will also be reviewed. Certain medical conditions, medications, or lifestyle factors such as smoking can affect the success of the implant. The dentist will discuss these factors with you to develop a personalized treatment plan. If any pre-existing conditions need to be addressed, such as gum disease or insufficient bone density, these will be managed before proceeding with the implant. Clear communication between you and your dentist during this phase is essential. You will have the opportunity to ask questions, discuss your expectations, and understand the risks and benefits associated with dental implants. This stage aims to ensure that you are fully informed and comfortable with the upcoming procedure.
The Implant Surgery
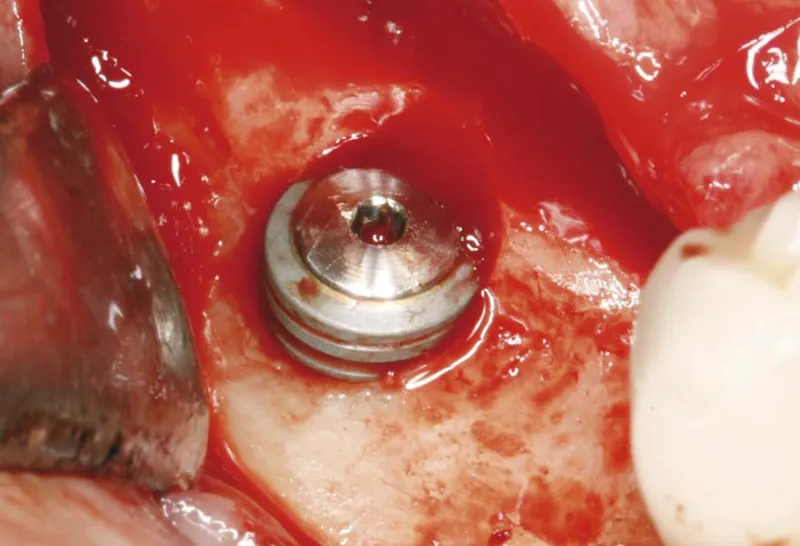
The actual implant surgery is typically an outpatient procedure performed under local anesthesia, though sedation options are available for those who may feel nervous. The first step involves making an incision in the gum to expose the jawbone. A specialized drill is then used to create space in the bone for the implant. The titanium implant, which acts as an artificial tooth root, is then carefully placed into this space. Once in place, the gum is stitched back over the implant.
After placing the implant, a period known as osseointegration begins. This is when the bone starts to grow around the implant, anchoring it firmly in place. Osseointegration is crucial for the stability and longevity of the implant and typically takes several months to complete. During this time, a temporary crown or denture may be placed to maintain aesthetics and function.
In some cases, additional procedures such as bone grafting or sinus lifts may be required to ensure there is enough bone to support the implant. These procedures are usually done prior to or during the implant surgery and help create a stable foundation for the implant. After osseointegration, a small connector known as an abutment is attached to the implant, which will hold the final crown in place.
Recovery and Aftercare
Recovery from dental implant surgery varies from patient to patient, but most people can expect some discomfort, swelling, and minor bleeding for a few days following the procedure. Your dentist will provide specific aftercare instructions, including pain management recommendations and tips for maintaining oral hygiene during the healing process. Adhering to these guidelines is crucial for preventing infection and ensuring successful healing.
Oral hygiene is particularly important after implant surgery. You will be advised to use a soft-bristled toothbrush and avoid the surgical site while brushing. Antibacterial mouth rinses may be recommended to keep the area clean. To promote healing, it is also essential to follow a balanced diet and avoid hard or chewy foods that could dislodge the implant.
Follow-up visits will be scheduled to monitor the healing process and assess the success of the implant. During these visits, any sutures may be removed, and the implant site will be checked for signs of proper osseointegration. Once the implant has fully integrated with the bone, the final restoration, such as a crown or bridge, can be placed.
In conclusion, understanding the dental implant procedure and the importance of each stage can help you make an informed decision about your oral health. The journey from initial consultation to full recovery may seem lengthy, but the result is a permanent solution that closely mimics the function and appearance of natural teeth. By following your dentist’s instructions and maintaining good oral hygiene, you can ensure the success and longevity of your dental implants.
If you found this article helpful, be sure to check out our other articles on related topics to further enhance your knowledge about dental health.
Cost Considerations
When considering dental implants and bone regeneration, understanding the cost implications is essential. Many patients are concerned about the potential expenses associated with these advanced dental procedures. This section aims to shed light on the various factors that influence costs and provide guidance on how to navigate insurance and financing options.
Dental implants and bone regeneration procedures are significant investments in one’s oral health, yet they offer long-term benefits that often outweigh the initial expenses. Knowing what to expect financially can help you make an informed decision and plan accordingly for these treatments.
Factors Influencing Cost
Several elements contribute to the overall cost of dental implants and bone regeneration procedures. Understanding these factors can help you anticipate expenses more accurately.
First, the complexity of the case plays a substantial role. More complicated procedures, such as those requiring extensive bone grafting or multiple implants, will generally be more expensive. Additionally, the quality of materials used for the implants, such as titanium or ceramic, can also affect the price.
Second, the expertise and experience of the dental professional performing the procedure can influence costs. Highly skilled implantologists or oral surgeons may charge higher fees, reflecting their specialized training and success rates.
Lastly, geographical location and the specific dental practice also impact costs. Dental clinics in metropolitan areas or regions with higher living costs may have higher fees compared to those in less populated areas.
Insurance Coverage
Insurance coverage for dental implants and bone regeneration can vary widely. It’s crucial to understand what your policy includes and the extent of coverage offered for these procedures.
Most standard dental insurance plans do not fully cover dental implants and bone regeneration since they are often considered elective or cosmetic procedures. However, some policies may offer partial coverage, especially if the procedure is deemed medically necessary due to trauma or congenital defects.
To maximize your benefits, consult with your insurance provider to get a clear understanding of your coverage. Ask about any pre-authorization requirements or necessary documentation to support your claim.
Additionally, some employers offer flexible spending accounts (FSAs) or health savings accounts (HSAs), which allow you to use pre-tax dollars to pay for qualified medical expenses, including dental procedures.
Financing Options
If your insurance does not cover the full cost of dental implants and bone regeneration, several financing options can help make these procedures more affordable.
Many dental practices offer payment plans, allowing patients to spread the cost over several months or even years. These plans can make it easier to manage the expense without compromising your budget.
Third-party financing companies, such as CareCredit or LendingClub, also provide specialized dental loans with flexible repayment terms. These loans often come with low or zero interest rates for a defined period, making them an attractive option for many patients. Another way to reduce costs is by exploring dental discount plans, which are membership-based programs offering reduced fees on various dental procedures. These plans can significantly lower your out-of-pocket expenses.
Understanding the cost considerations for dental implants and bone regeneration is just the beginning. We invite you to delve deeper into related topics to help you make the best decisions for your oral health. Explore our other articles to learn more about treatment options, recovery processes, and the latest advancements in dental technology.
Dental implants: Everything you need to know before deciding
If you are considering dental implants, it is essential to gather as much information as possible before making a decision. Here are some frequently asked questions that might help you understand more about this procedure.
What are dental implants and how do they work?
Dental implants are artificial tooth roots, typically made from titanium, that are surgically placed into the jawbone. Over time, they integrate with the bone, providing a stable foundation for replacement teeth such as crowns, bridges, or dentures. This integration process, known as osseointegration, ensures that the implant remains securely anchored in the jaw, providing functionality and appearance similar to natural teeth.

My name is Salman Kapa, a 73-year-old expert in bone regeneration and dental implantology. With decades of experience in the field, I am dedicated to advancing our understanding of oral health and hygiene. Through my research and writing, I aim to contribute to the development of innovative solutions in dental care.