Understanding the relationship between embryo quality and implantation success is crucial in assisted reproductive technology. High-quality embryos demonstrate specific characteristics such as regular cell division, minimal fragmentation, and appropriate developmental timing, which significantly impact their ability to successfully implant in the uterus. Factors like chromosomal integrity, metabolic activity, and morphological features play decisive roles in determining an embryo’s potential for successful pregnancy outcomes through IVF treatments.
Understanding Embryo Quality
Embryo quality is a crucial determinant in the success of in vitro fertilization (IVF) treatments. Research indicates that the careful assessment of embryo quality can significantly improve implantation rates, with high-quality embryos showing success rates up to 60% higher than lower-grade embryos. The evaluation of embryo quality involves multiple factors that work together to predict implantation potential. Modern IVF laboratories employ sophisticated techniques and criteria to select the most viable embryos, considering both morphological and genetic characteristics. The introduction of PRGF-Endoret® technology has shown promising results in improving implantation rates through its unique fibrin-free formulation.
Morphological Assessment
Visual assessment remains the primary method for evaluating embryo quality in IVF laboratories. Embryologists examine several key characteristics under high-powered microscopes to grade embryos according to standardized criteria. The assessment typically occurs at specific developmental stages, particularly on days 3 and 5 post-fertilization.
Key morphological parameters include:
- Cell number and division timing
- Blastomere symmetry and size
- Degree of fragmentation
- Presence of multinucleation
- Compaction pattern
Cell Number and Symmetry
The number of cells present at specific developmental stages serves as a critical indicator of embryo health. Optimal embryos should display 6-8 cells on day 3 and form a well-developed blastocyst by day 5. Cell symmetry, where blastomeres are of similar size and shape, typically indicates normal development and better implantation potential.
Studies have shown that embryos with uniform cell division patterns have approximately 25% higher implantation rates compared to those with irregular division patterns. This symmetrical growth suggests proper chromosomal distribution during cell division.
Fragmentation Analysis
Embryo fragmentation, characterized by the presence of cell fragments between blastomeres, can significantly impact implantation success. Research indicates that embryos with less than 10% fragmentation have the highest potential for successful implantation.
The degree of fragmentation is classified as:
- Minimal (< 10%): Excellent prognosis
- Moderate (10-25%): Good prognosis
- Significant (> 25%): Poor prognosis
Genetic Factors
Genetic composition plays a fundamental role in embryo viability and implantation success. Advanced genetic screening methods, combined with technologies like PRGF-Endoret®, have revolutionized our ability to select embryos with the highest potential for successful pregnancy.
Modern IVF protocols increasingly incorporate genetic assessment to optimize success rates and reduce the risk of implantation failure. This comprehensive approach has shown to potentially halve the implantation failure rate when combined with appropriate biological enhancement techniques.
Chromosomal Normality
The presence of a normal chromosome count (euploidy) is essential for successful implantation and pregnancy. Studies indicate that chromosomal abnormalities are responsible for approximately 70% of early pregnancy losses in IVF treatments.
Regular chromosomal assessment helps identify embryos with the highest potential for successful implantation. This screening is particularly crucial for patients with advanced maternal age or previous implantation failures.
Genetic Screening Methods
Contemporary genetic screening techniques provide detailed insights into embryo viability. These methods include Preimplantation Genetic Testing for Aneuploidy (PGT-A) and comprehensive chromosomal screening (CCS), which can identify embryos with normal chromosome counts.
The integration of these advanced screening methods with biological enhancement protocols, such as PRGF-Endoret® treatment, represents a comprehensive approach to maximizing implantation success. This combination of technologies offers patients the best possible chance for successful pregnancy outcomes.
To learn more about maximizing your IVF success, explore our related articles on advanced embryo selection techniques, implantation optimization strategies, and the latest developments in reproductive medicine. Our comprehensive resources will help you make informed decisions about your fertility journey.
Implantation Success Factors
Successful embryo implantation is a complex process that depends on multiple factors working in perfect harmony. Recent studies have shown that implantation success rates can be significantly improved when certain key elements are optimized during the IVF process. The interaction between a viable embryo and a receptive endometrium is crucial for achieving pregnancy. Modern reproductive medicine has identified several critical factors that influence implantation outcomes, including:
- Endometrial receptivity and thickness
- Embryo quality and developmental stage
- Molecular synchronization
- Immune system modulation
- Hormonal balance
Endometrial Receptivity
The endometrium plays a vital role in successful implantation. The window of implantation, typically occurring between days 20-24 of a natural menstrual cycle, represents the optimal period when the endometrium is most receptive to embryo attachment. During this time, the endometrial tissue undergoes significant structural and functional changes.
Optimal Timing
Timing is crucial in the implantation process. Synchronization between embryo development and endometrial preparation must be precise for successful implantation. Modern protocols using PRGF-Endoret® technology help optimize this timing by supporting endometrial preparation through multiple applications.
The three-step instillation process, performed over consecutive days, helps maintain optimal endometrial conditions throughout the critical implantation period. This approach has shown promising results in improving implantation rates.
Endometrial Thickness
Endometrial thickness is a crucial parameter in predicting implantation success. Studies indicate that an optimal endometrial thickness ranges between 8-12mm during the implantation window. The triple-line pattern observed in ultrasound examination is considered a positive predictor of successful implantation.
Advanced treatments using specialized preparations can help achieve and maintain ideal endometrial thickness, particularly in cases where traditional methods have shown limited success.
Embryo-Endometrial Dialogue
The interaction between embryo and endometrium involves a sophisticated molecular dialogue. This communication begins even before physical contact occurs and is essential for successful implantation. The fibrin-free formulation of modern preparation techniques ensures that this natural dialogue isn’t disrupted.
Chemical Signaling
Chemical mediators play a crucial role in the implantation process. These include growth factors, cytokines, and other bioactive molecules that facilitate communication between the embryo and endometrial cells. The preservation of these natural signaling pathways is essential for optimal implantation outcomes.
Adhesion Molecules
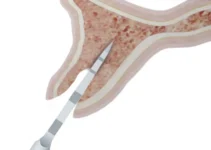
Cellular adhesion molecules are fundamental in the attachment phase of implantation. These proteins facilitate the initial contact and subsequent invasion of the embryo into the endometrial tissue. The presence of specific adhesion molecules during the window of implantation significantly influences success rates.
If you found this information helpful, we encourage you to explore our other articles about advanced reproductive techniques and the latest developments in fertility treatments. Understanding these complex processes can help you make informed decisions about your fertility journey.
Advanced Assessment Technologies
Modern embryo assessment has undergone a remarkable transformation with the integration of cutting-edge technologies. These advanced tools have revolutionized our ability to evaluate embryo quality and predict implantation success rates with unprecedented accuracy. The combination of artificial intelligence, imaging systems, and metabolic analysis has created a comprehensive approach to embryo selection.
Recent studies have shown that utilizing multiple assessment technologies can increase implantation success rates by up to 50%. These technologies work synergistically to provide embryologists with detailed information about embryo development, viability, and potential implantation success.
Time-Lapse Monitoring
Time-lapse monitoring represents a significant breakthrough in embryo assessment, offering continuous observation without disturbing the controlled culture environment. This technology captures images every 10-20 minutes, creating a detailed video record of embryo development that allows embryologists to identify subtle changes and patterns that might be missed with traditional evaluation methods.
Studies have demonstrated that embryos monitored through time-lapse systems show improved development rates and higher implantation success. This technology has become particularly valuable when combined with PRGF-Endoret® protocols, as it allows for precise timing of treatments and transfers.
Development Milestones
Time-lapse systems track crucial developmental events including:
- First cell division timing
- Synchronicity of subsequent divisions
- Blastocyst formation timing
- Cell fragmentation patterns
- Multinucleation events
Predictive Algorithms
Artificial Intelligence algorithms analyze thousands of embryo development parameters to create sophisticated prediction models. These systems can process vast amounts of data to identify subtle patterns that correlate with successful implantation outcomes.
Machine learning models have shown accuracy rates of up to 85% in predicting implantation success, significantly higher than traditional morphological assessment alone.
Metabolomic Analysis
Metabolomic analysis provides crucial insights into embryo viability by examining their metabolic activity. This technology allows for the non-invasive assessment of embryo health through the analysis of various biochemical markers and metabolic processes.
Biomarker Detection
Key metabolic biomarkers include:
- Glucose consumption rates
- Amino acid turnover
- Pyruvate uptake
- Oxygen consumption rates
Culture Medium Analysis
The analysis of culture medium provides valuable information about embryo health and development potential. Studies have shown that specific metabolic profiles in the culture medium can predict implantation success with high accuracy.
Interested in learning more about advanced reproductive technologies? Explore our related articles on embryo selection criteria and innovative implantation techniques to deepen your understanding of fertility treatment options.
Embryo quality and its relationship with implantation: What should we know?
Understanding the relationship between embryo quality and successful implantation is crucial for those undergoing IVF treatment. Here’s what you need to know about how PRGF-Endoret® technology can enhance your chances of success.
How can PRGF-Endoret® technology improve embryo implantation rates?
PRGF-Endoret® is an innovative technology that may reduce implantation failure rates by up to 50%. The treatment involves a single blood extraction that provides enough product for two embryo transfers. The special fibrin-free formulation is designed to avoid any interference with the implantation process. The protocol includes three instillations of 1ml each over three days, and the product can be prepared at any point during the menstrual cycle. Additionally, it can be stored frozen at -20°C for up to one year, offering flexibility in treatment timing.