Mouth breathing can significantly impact oral and overall health, influencing everything from gum disease to orthodontic problems. Habitual mouth breathers often experience dry mouth, which reduces the saliva flow necessary to protect teeth from decay and gums from infection. Additionally, this habit might lead to more severe health issues like sleep apnea and poor oxygen concentration. Understanding the implications of mouth breathing is crucial for prevention and managing potential harm, emphasizing the need for awareness and proactive oral care strategies.
What is a Mouth Breather?
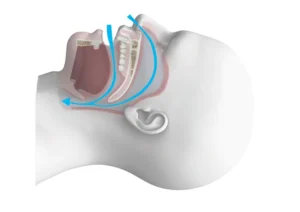
Breathing is an essential function of life, with the nose and mouth serving as the primary pathways for air intake. Yet, some individuals predominantly breathe through their mouths rather than their noses, a phenomenon commonly referred to as “mouth breathing.” A mouth breather is someone who consistently inhales and exhales through their mouth instead of their nasal passages. This behavior can be due to various reasons, including nasal obstructions, allergies, or habit. Proper nasal breathing is crucial for several physiological reasons, such as filtering and humidifying the air before it reaches the lungs. Consequently, habitual mouth breathing can lead to several health issues and complications over time.
Mouth breathing can be categorized into two main types: obstructive mouth breathing and habitual mouth breathing. Obstructive mouth breathing occurs when an anatomical or pathological obstruction in the nasal passages prompts the individual to breathe through their mouth. Common causes include enlarged adenoids, nasal polyps, or chronic sinusitis. On the other hand, habitual mouth breathing develops when there is no physical obstruction, but the person has developed the habit of mouth breathing, often starting from childhood.
Numerous studies have demonstrated that mouth breathing can have significant impacts on oral health, facial development, and even cognitive function. Chronic mouth breathing can lead to dry mouth (xerostomia), which increases the risk of dental cavities and oral infections. Furthermore, it can cause alterations in facial growth, leading to a condition known as “adenoid facies,” characterized by an elongated face, open bite, and narrow palate. Understanding the causes, implications, and treatments for mouth breathing is vital for overall health and well-being.
Effects of Mouth Breathing on Oral Health
Mouth breathing is often overlooked as a minor inconvenience, but it can have significant repercussions on overall oral health. The prevalence of mouth breathing, especially during sleep, can lead to a variety of dental and medical conditions that may require intervention by healthcare professionals. Understanding the risks and implementing preventive measures is crucial for maintaining optimal oral health.
Mouth breathing can be caused by several factors, including nasal obstructions, allergies, or anatomical irregularities. It is essential to address the root cause to mitigate the potential adverse effects on oral health. This section explores the various ways in which mouth breathing can impact your oral health, focusing on dry mouth, gum disease, and tooth decay.
Dry Mouth and Its Consequences
One of the most immediate effects of mouth breathing is dry mouth (xerostomia). When you breathe through your mouth, the saliva that normally helps to cleanse and protect your oral cavity evaporates more quickly. This can create an environment in which bacteria thrive, leading to a host of dental problems.
Dry mouth can result in a range of unpleasant symptoms, including bad breath, difficulty swallowing, and an increased risk of oral infections. Saliva is essential because it neutralizes acids produced by bacteria in the mouth, limiting the growth of harmful microorganisms. Without sufficient saliva, the oral cavity becomes more susceptible to decay and disease.
Moreover, prolonged dry mouth can contribute to the formation of mouth sores and an altered sense of taste. Regular hydration, the use of saliva substitutes, and addressing the underlying causes of mouth dryness can help mitigate these effects.
Increased Risk of Gum Disease
Mouth breathing can also increase the risk of developing gum disease, or periodontal disease. Healthy gums serve as a barrier against bacterial infection, but when the mouth is dry, this barrier can be compromised. A lack of saliva means that food particles and bacteria are not effectively washed away, increasing the likelihood of plaque buildup.
Gum disease starts with gingivitis, characterized by red, swollen, and bleeding gums. If left untreated, it can progress to periodontitis, a more severe condition that can lead to tooth loss and damage to the jawbone. The inflammatory response triggered by bacterial accumulation can harm the supporting structures of the teeth, making early detection and management critical. Maintaining good oral hygiene, including regular brushing and flossing, and seeking professional dental care can help prevent gum disease. Additionally, addressing the root causes of mouth breathing can significantly reduce the risk of periodontal issues.
Tooth Decay and Mouth Breathing
The relationship between mouth breathing and tooth decay is well-documented. When the mouth is consistently dry, the decreased saliva flow reduces the natural remineralization process of the teeth, making them more prone to cavities. Saliva not only helps to wash away food particles but also contains enzymes that aid in the repair of enamel.
Individuals who breathe through their mouth may notice an increase in dental caries, particularly along the gumline and on the surfaces of the teeth that are less exposed to saliva. This is because the protective role of saliva is compromised, leading to frequent acid attacks on the enamel and dentin.
Preventative strategies include using fluoride toothpaste, consuming a balanced diet low in sugar, and undergoing regular dental check-ups to monitor and address any early signs of decay. Addressing mouth breathing through medical or surgical interventions, such as treating nasal obstructions or using dental appliances, can also be beneficial.
In conclusion, mouth breathing can have a profound impact on oral health, leading to dry mouth, increased risk of gum disease, and heightened susceptibility to tooth decay. It’s important to identify and address the underlying causes of mouth breathing to mitigate these effects. If you found this article insightful, consider reading our other articles on dental health for more comprehensive information.
Solutions for Mouth Breathing
Mouth breathing, a common issue often overlooked, can lead to a variety of dental and health problems. It’s critical to understand and address the root causes of mouth breathing to improve overall health and well-being. Solutions to this issue range from simple techniques to more advanced medical interventions, depending on the underlying causes.
Addressing mouth breathing effectively involves a multidisciplinary approach. Sometimes, lifestyle changes and exercises can mitigate the problem, while other times, professional medical treatments are necessary. By exploring different solutions, individuals can find the method that best suits their specific needs.
Let’s delve into some of the most effective solutions for mouth breathing, including specific nasal breathing techniques and medical interventions that can help restore proper nasal function and improve quality of life.
Nasal Breathing Techniques
One of the most natural and effective ways to combat mouth breathing is by practicing nasal breathing techniques. These exercises help to open the nasal passages, encouraging air to flow through the nose rather than the mouth. Nasal breathing has numerous benefits, such as filtering and humidifying the air before it reaches the lungs, which is essential for overall respiratory health.
One common technique is the “Buteyko breathing method,” which focuses on reducing breathing volume to help decongest the nose. This method involves slowing down the breath and holding it momentarily, which can lead to an increase in carbon dioxide levels in the blood and help open the nasal passages. Studies have shown that this technique can be particularly effective in reducing symptoms of asthma and other respiratory issues.
Another useful exercise is nasal irrigation, commonly known as using a neti pot. This traditional practice involves pouring saline solution through one nostril and allowing it to flow out the other, effectively clearing out any blockages and mucus. This method not only improves nasal passage function but also reduces the risk of infections.
Additionally, practicing diaphragmatic breathing, where breath control is centered in the diaphragm rather than the chest, can help promote nasal breathing. This technique encourages deeper and more controlled breaths, which can prevent the tendency to mouth breathe.
Medical Interventions
While breathing techniques can be highly effective, there are cases where medical interventions are necessary to address more severe or underlying issues. For instance, chronic nasal obstruction caused by a deviated septum, nasal polyps, or enlarged turbinates may require surgical correction. Procedures like septoplasty or turbinate reduction can significantly improve nasal airflow. Another medical intervention is the use of Continuous Positive Airway Pressure (CPAP) therapy for individuals with obstructive sleep apnea (OSA). OSA is a condition where the airway collapses during sleep, leading to breathing pauses and often resulting in mouth breathing. CPAP machines help keep the airway open by providing a continuous stream of air, thus encouraging nasal breathing.
Allergy management is also a crucial aspect of addressing mouth breathing. Allergies can cause nasal congestion and inflammation, making it difficult to breathe through the nose. Treatments may include antihistamines, nasal corticosteroids, or immunotherapy to reduce allergic reactions and improve nasal airflow.
In some cases, orthodontic treatments like expanders or braces are necessary to address structural issues in the mouth and jaw that contribute to mouth breathing. By correcting these structural problems, individuals can achieve better nasal airflow and overall breathing function.
Exploring these solutions can significantly improve quality of life by ensuring proper breathing patterns. For more information on improving your dental and overall health, be sure to check out our other articles on related topics.
Frequently Asked Questions About Mouth Breathing
Many people have questions about the implications of mouth breathing on oral health. Here’s a common inquiry:
What are the dental health risks associated with being a mouth breather?
Mouth breathing can lead to several dental health issues, including dry mouth, which reduces saliva production necessary for neutralizing acids and washing away food particles. This can increase the risk of tooth decay and gum disease. Moreover, mouth breathing may also lead to orthodontic problems like an altered jaw position and abnormal facial development, commonly referred to as “long face syndrome.”

My name is Salman Kapa, a 73-year-old expert in bone regeneration and dental implantology. With decades of experience in the field, I am dedicated to advancing our understanding of oral health and hygiene. Through my research and writing, I aim to contribute to the development of innovative solutions in dental care.