Understanding how to prevent drug-associated osteonecrosis of the jaws (ONJ) is crucial for patients undergoing treatments that increase the risk of this severe condition. ONJ can result from the use of medications such as bisphosphonates, primarily used to treat osteoporosis and certain cancers. Prevention strategies include good oral hygiene, regular dental check-ups, and the careful management of medication dosages. It’s important for patients to be aware of the initial symptoms, such as pain or numbness in the jaw, to seek timely treatment. This article discusses methods to effectively reduce the risk and ensure better oral health outcomes for at-risk individuals.
Overview of Drug-Associated Osteonecrosis of the Jaws
Drug-associated osteonecrosis of the jaws (ONJ) is a severe condition characterized by the death of bone tissue in the jaw. It is primarily linked to the use of specific medications, such as bisphosphonates and antiresorptive drugs, which are commonly prescribed for the treatment of osteoporosis, metastatic cancers, and other bone diseases. Understanding the etiology, symptoms, and risk factors associated with ONJ is crucial for its prevention and management. ONJ can significantly impact a patient’s quality of life, causing pain, infection, and eventually leading to the loss of jaw function if not properly managed. The condition is often difficult to treat and can present challenges even for experienced dental professionals. Therefore, a comprehensive understanding of the condition, including meticulous patient assessment and preventive strategies, is essential for effective management.
In this article, we will delve into the definition, causes, symptoms, diagnosis, and risk factors of drug-associated osteonecrosis of the jaws. Our goal is to provide a thorough overview that will aid both clinicians and patients in recognizing and managing this complex condition effectively.
Definition and Causes
Drug-associated osteonecrosis of the jaws (ONJ) is defined as the exposure of jawbone through the oral mucosa, persisting for more than eight weeks, in patients who have been treated with antiresorptive or antiangiogenic medications but have not received radiation therapy to the craniofacial region. This condition is primarily linked to medications like bisphosphonates, denosumab, and certain chemotherapeutic agents.
The primary cause of ONJ is believed to be the inhibition of bone remodeling. Medications like bisphosphonates and denosumab suppress osteoclast activity, leading to reduced bone turnover. This can result in the accumulation of microdamage within the bone and the subsequent development of necrosis. Moreover, these drugs can also impair angiogenesis, further exacerbating the risk of bone necrosis.
Additional factors such as dental extractions, trauma to the jawbone, and poor oral hygiene can contribute to the development of ONJ. For instance, patients undergoing invasive dental procedures are at a higher risk due to the direct impact on jawbone integrity. Understanding these contributing factors is essential for both prevention and management of the condition.
Symptoms and Diagnosis
The symptoms of drug-associated osteonecrosis of the jaws can vary but generally include pain, swelling, and the presence of exposed bone. In some cases, patients may experience numbness or a “heavy” feeling in the jaw. Other signs can include infection, loosening of teeth, and drainage of pus. Early identification of these symptoms is crucial for timely intervention and management.
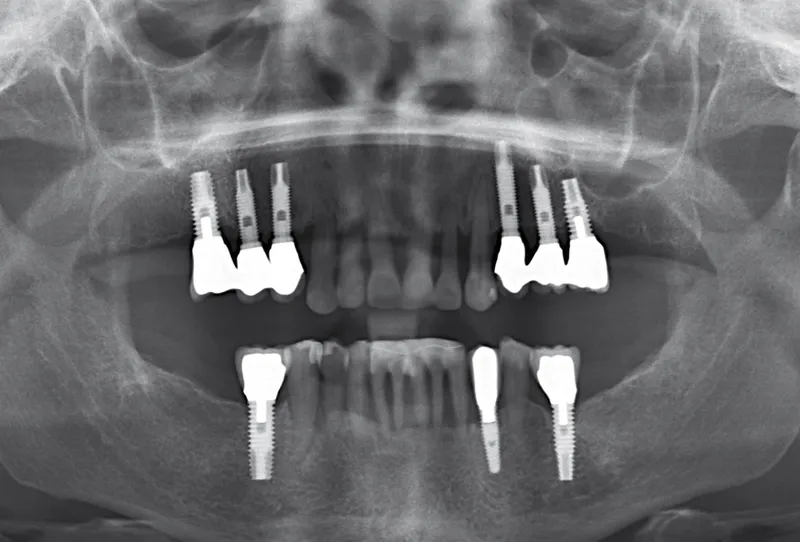
Diagnosis of ONJ typically involves a combination of clinical examination and imaging studies. Dentists often rely on visual inspection to identify exposed bone and assess for signs of infection. Radiographic imaging, such as panoramic X-rays and CT scans, can help in determining the extent of bone involvement and identifying areas of necrosis that are not superficially visible.
In specific circumstances, a biopsy may be performed to rule out other conditions that may mimic the symptoms of ONJ, such as osteomyelitis or malignancies. Accurate diagnosis is critical as it dictates the appropriate course of treatment and preventive measures.
 Identifying ONJ in its early stages can significantly enhance treatment outcomes and improve the patient’s quality of life. Therefore, both patients and healthcare providers should be vigilant about monitoring for early signs and symptoms of this condition, especially in those undergoing treatment with high-risk medications.
Identifying ONJ in its early stages can significantly enhance treatment outcomes and improve the patient’s quality of life. Therefore, both patients and healthcare providers should be vigilant about monitoring for early signs and symptoms of this condition, especially in those undergoing treatment with high-risk medications.
Risk Factors
Several risk factors are associated with the development of drug-associated osteonecrosis of the jaws. These can be broadly categorized into medication-related, patient-related, and procedure-related factors. Understanding these risk factors helps in stratifying patients who may be at higher risk and implementing necessary preventive measures.
- Medication-related factors: The type, dosage, and duration of medication play a crucial role in the development of ONJ. High doses of bisphosphonates or prolonged use of antiresorptive drugs significantly increase the risk.
- Patient-related factors: Poor oral hygiene, pre-existing dental conditions, and systemic diseases such as diabetes can elevate the risk of developing ONJ. Additionally, elderly patients are generally at a higher risk due to slower bone healing processes.
- Procedure-related factors: Invasive dental procedures like tooth extractions or dental implants can predispose patients to ONJ. Trauma to the jawbone, whether from surgical procedures or ill-fitting dentures, can also contribute to the risk.
Preventive strategies such as maintaining excellent oral hygiene, routine dental check-ups, and minimizing invasive dental procedures during medication use can significantly reduce the risk of ONJ. Patient education and multi-disciplinary collaboration between dentists, oncologists, and other healthcare providers are essential in preventing and managing drug-associated osteonecrosis of the jaws effectively.
By recognizing and addressing these risk factors, healthcare providers can reduce the incidence of ONJ and improve the overall prognosis for patients at risk. For further information on related topics, consider exploring additional articles on our website, which delve into the latest research and treatment options available in the field.
Preventive Measures
Maintaining oral health is essential for preventing dental complications and preserving the longevity of both natural and prosthetic teeth. Preventive measures are key to reducing the likelihood of needing complex procedures such as dental implants or bone regeneration. This section discusses the importance of dental hygiene, regular checkups, medication management, and surgical interventions to keep your oral health in check.
An effective preventive strategy incorporates not only personal habits but also professional medical advice. These measures ensure that common dental problems are caught early and managed appropriately. Let’s explore the various preventive measures that are essential for maintaining optimal oral health.
Dental Hygiene and Regular Checkups
Good dental hygiene practices are the cornerstone of oral health. Brushing your teeth at least twice a day with fluoride toothpaste, flossing daily, and using mouthwash can eliminate harmful bacteria and food particles from the mouth. These practices help prevent the buildup of plaque and tartar, which can lead to tooth decay and gum disease.
Regular dental checkups are equally crucial. Visiting your dentist every six months allows for early detection of potential issues. Professional cleanings remove tartar that cannot be eliminated with regular brushing and flossing. Your dentist can also take X-rays to detect hidden problems, such as tooth decay between teeth or issues beneath the gums.
Consider the following benefits of regular dental checkups:
- Early detection of oral cancers
- Prevention of gum disease
- Maintenance of overall oral health
- Personalized oral care advice
Medication Management
Your oral health can be significantly affected by certain medications you may be taking. Some drugs can cause dry mouth, which increases the risk of cavities and gum disease. Others might lead to gum overgrowth or interactions with commonly used dental anesthetics.
Patients should inform their dentist about all the medications and supplements they are taking. This information helps the dentist to provide a comprehensive treatment plan that accommodates these variables. Medications to watch out for include:
- Antihistamines
- Antidepressants
- Blood pressure medications
- Cancer treatments
Managing your medication effectively can mitigate side effects that compromise oral health. Your dentist may recommend saliva substitutes or special mouthwashes to combat dry mouth or other issues caused by medication.
Surgical Interventions
In some cases, more proactive surgical interventions may be necessary to prevent further oral health problems. For instance, scaling and root planing, which involves deep cleaning of the gums, can help treat early stages of gum disease. If gum disease is more advanced, flap surgery might be necessary to clean the roots of the teeth and repair bone damage.
For patients requiring dental implants, ensuring that the jawbone is strong enough to support the implant is crucial. Bone grafting is a common surgical intervention used to augment the jawbone. This procedure ensures there is sufficient bone density and volume to support the implant securely. Other surgical preventive measures may include:
- Soft tissue grafts to prevent gum recession
- Cyst or tumor removal
- Tooth extractions to prevent overcrowding or remove problematic teeth
Surgical interventions, while more invasive, play a vital role in maintaining oral health and preventing future complications. They can provide long-term solutions that significantly improve your quality of life.
By adopting these preventive measures, you can maintain excellent oral health and avoid the need for more complex dental procedures. For more in-depth information on dental health and advanced treatments, make sure to read our other articles on these subjects.
Patient Education and Awareness
Patient education and awareness are fundamental components of dental implantology and bone regeneration. By educating patients, we can significantly improve outcomes, reduce anxiety, and enhance patient compliance. Informed patients are more likely to engage in their treatment plans and make decisions that support their long-term dental health.
Effective patient education encompasses various facets, from explaining the procedures to addressing concerns and providing post-operative care instructions. It is crucial in ensuring that patients understand the importance of maintaining their oral health, the benefits of dental implants, and the impact of bone regeneration techniques.
Importance of Patient Education
Educating patients about dental implant procedures and bone regeneration is vital for several reasons. First and foremost, it helps mitigate fear and anxiety. Many patients experience apprehension about dental surgeries, but providing detailed information about what to expect can alleviate these concerns. Studies have shown that patients who are well-informed about their procedures experience lower levels of anxiety and have better post-operative outcomes.
Moreover, patient education ensures better compliance with pre- and post-operative instructions, which are critical for the success of dental implants. When patients understand the importance of following guidelines, they are more likely to adhere to them, reducing the risk of complications. This includes maintaining oral hygiene, attending follow-up appointments, and avoiding certain activities that might jeopardize their recovery.
Finally, patient education fosters better communication between the dentist and the patient. When patients are well-informed, they are more likely to ask relevant questions and express their concerns. This open dialogue helps create a trusting relationship, making it easier to tailor treatments to the individual needs of each patient.
Resources for Patients
Providing patients with accessible and comprehensive resources is essential to their education. These resources can come in various forms, including brochures, videos, websites, and one-on-one consultations. High-quality educational materials help patients understand complex procedures and the science behind bone regeneration and dental implants.
1. Brochures and Handouts: These can be given during consultations or sent home with patients. They should include detailed information about the procedures, what to expect, and how to prepare for surgery.2. Videos: Visual aids are particularly effective in explaining procedures. Videos can demonstrate the steps involved in dental implant surgery and bone regeneration, making it easier for patients to grasp the concepts.3. Websites: A well-organized website can serve as a comprehensive resource for patients. It can include articles, FAQs, and interactive tools like virtual consultations or appointment scheduling.4. Consultations: One-on-one consultations provide an opportunity for personalized education. During these sessions, patients can ask questions and receive detailed answers tailored to their specific concerns and conditions.
Furthermore, referring patients to reputable sources such as professional dental associations can enhance their understanding. Encouraging patients to seek information from credible sources ensures they receive accurate and reliable data. This approach helps build their confidence and trust in the treatment process.
At the end of the day, patient education is not just about conveying information; it’s about empowering patients to take an active role in their dental care. By leveraging various resources and techniques, we can ensure that our patients are well-informed and prepared for their treatment journeys.
If you found this article helpful, be sure to check out our other articles on dental health, implant care, and advances in oral surgery to continue expanding your knowledge.
Clinical Recommendations
In the field of implant dentistry, clinical recommendations are based on evidence-backed research and best practices to ensure successful outcomes for patients. Implantology and bone regeneration have evolved significantly over the years, offering enhanced techniques and materials for improved patient care. Clinicians must stay updated with the latest guidelines to provide optimal treatment.
Adhering to clinical guidelines not only increases the success rate of implant procedures but also minimizes the risk of complications. It is essential to follow a systematic approach that includes thorough patient evaluation, meticulous surgical planning, and the use of high-quality implant materials. Regular follow-ups and patient education play a crucial role in the long-term success of implants.
Guidelines for Healthcare Providers
Healthcare providers must adopt a comprehensive treatment strategy when dealing with implantology and bone regeneration. The first step involves a detailed patient assessment, including medical history, oral examinations, and radiographic analysis. This helps in identifying potential risk factors such as systemic conditions, smoking habits, or poor oral hygiene that could affect the success of the implant.
Once the assessment is completed, providers should focus on surgical planning. This involves selecting the appropriate implant type, size, and placement site, considering the patient’s anatomical structure and bone quality. Advanced imaging techniques, such as cone-beam computed tomography (CBCT), can provide valuable insights for precise planning.
During the surgical phase, emphasizing a sterile environment and using minimally invasive techniques can significantly reduce the risk of complications. The choice of biomaterials for bone grafting or regenerative procedures should be based on their biocompatibility and osteoconductive properties.
- Use of autografts, allografts, or xenografts as per the patient’s needs
- Application of growth factors and biologic agents to enhance bone regeneration
- Monitoring for signs of infection or graft rejection
Post-operative care is equally important. Providers should guide patients on maintaining oral hygiene, managing post-surgical pain, and recognizing early signs of complications. Regular follow-up appointments are necessary to monitor the healing process and the stability of the implant.
By adhering to these guidelines, healthcare providers can significantly improve patient outcomes in implantology and bone regeneration. For more detailed information on advanced techniques and case studies, explore our other articles on related topics.
Key Questions on Preventing Drug-Associated Osteonecrosia of the Jaws
This section addresses common inquiries about preventing the serious condition of osteonecrosis of the jaws associated with certain drugs, offering clear, concise information.
What are the main strategies for preventing drug-associated osteonecrosis of the jaws?
To prevent osteonecrosis of the jaws, which can occur after the use of medications like bisphosphonates and denosumab (often prescribed for cancer treatment or osteoporosis), it’s crucial to maintain excellent oral hygiene, routinely visit your dentist, especially before starting such medications, and avoid invasive dental procedures whenever possible during treatment. Patients should also inform their dentist about their medication history to tailor preventative care precisely.

My name is Salman Kapa, a 73-year-old expert in bone regeneration and dental implantology. With decades of experience in the field, I am dedicated to advancing our understanding of oral health and hygiene. Through my research and writing, I aim to contribute to the development of innovative solutions in dental care.