Sleep apnea, a condition marked by repeated interruptions in breathing during sleep, can be significantly influenced by the tonsils. These lymphatic tissues, located at the back of the throat, can become enlarged and obstruct the airway, particularly in children. This obstruction contributes to obstructive sleep apnea (OSA), where the airflow stops despite ongoing effort to breathe. Understanding how tonsils impact sleep apnea is crucial for diagnosing and managing this condition effectively. Treatments may include lifestyle changes, medical interventions, or in some cases, surgical removal of the tonsils to restore normal breathing patterns during sleep.
Understanding Sleep Apnea
Sleep apnea is a serious sleep disorder that affects millions of people worldwide. This condition is characterized by repeated interruptions in breathing during sleep, which can lead to fragmented sleep and reduced oxygen levels in the blood. Understanding sleep apnea is crucial for recognizing its symptoms and seeking appropriate treatment. 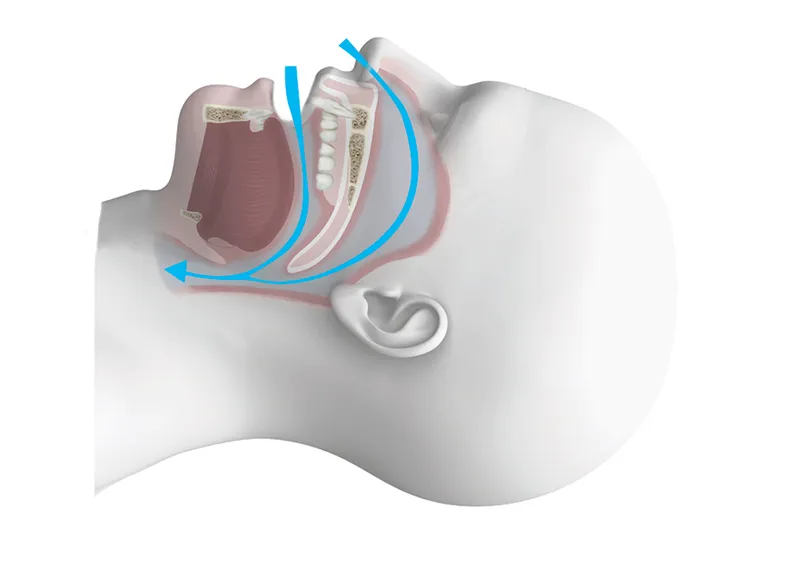
In addition to disturbing your sleep, sleep apnea can have severe health consequences, including an increased risk of cardiovascular diseases, stroke, hypertension, and diabetes. By learning more about the nature of sleep apnea and its types, individuals can be better equipped to manage this condition effectively.
Definition of Sleep Apnea
Sleep apnea is defined as a condition in which an individual’s breathing repeatedly stops and starts during sleep. The word “apnea” is derived from the Greek word “apnoea,” meaning “without breath.” These episodes of disrupted breathing can last anywhere from a few seconds to over a minute and can occur multiple times throughout the night. During an apnea event, the body’s oxygen levels drop, and carbon dioxide levels rise, triggering the brain to wake the person briefly to resume normal breathing. These awakenings are often so brief that they go unnoticed, but they can significantly disrupt the sleep cycle and lead to excessive daytime sleepiness and other related issues.
Doctors usually diagnose sleep apnea using polysomnography, an overnight sleep study that monitors various physiological functions, including brain activity, eye movement, muscle activity, heart rhythm, and breathing patterns. Understanding the definition and diagnosis of sleep apnea is the first step toward effective management and treatment.
Types of Sleep Apnea
There are three main types of sleep apnea: obstructive sleep apnea (OSA), central sleep apnea (CSA), and complex sleep apnea syndrome (CompSAS), also known as treatment-emergent central sleep apnea. Each type has distinct causes and characteristics.
1. Obstructive Sleep Apnea (OSA): This is the most common form of sleep apnea. It occurs when the muscles at the back of the throat relax excessively, causing a blockage in the airway. As a result, the person experiences a temporary cessation of breathing. OSA is often associated with factors such as obesity, enlarged tonsils, and structural abnormalities in the airway.
2. Central Sleep Apnea (CSA): Unlike OSA, CSA is not caused by a physical blockage of the airway. Instead, it occurs when the brain fails to send proper signals to the muscles that control breathing. This type of sleep apnea is less common and is often linked to medical conditions such as heart failure, stroke, or use of certain medications.
3. Complex Sleep Apnea Syndrome (CompSAS): Also known as treatment-emergent central sleep apnea, CompSAS is a combination of both OSA and CSA. It typically appears in individuals who are initially diagnosed with obstructive sleep apnea and begin treatment with continuous positive airway pressure (CPAP) therapy, only to develop central sleep apnea symptoms later.
Identifying the type of sleep apnea is essential for determining the most effective treatment approach. Each type may require different management strategies, ranging from lifestyle changes and the use of CPAP machines to surgical interventions.
For more detailed information on treatment options, lifestyle modifications, and advanced research in the field of sleep apnea, be sure to explore our other articles dedicated to this critical subject.
The Role of Tonsils in Sleep Apnea
The tonsils, two masses of tissue located at the back of the throat, play a significant role in the immune system by acting as a first line of defense against infection. Despite their crucial function, the tonsils can sometimes become a source of health issues, particularly in relation to sleep apnea. Sleep apnea is a potentially serious disorder where breathing repeatedly stops and starts during sleep, and enlarged tonsils are a common underlying cause, especially in children.
Understanding the correlation between enlarged tonsils and sleep apnea is vital for both diagnosing and treating this condition. When the tonsils are enlarged, they can obstruct the airway, making it difficult to breathe normally during sleep. This can lead to a variety of health problems, including disrupted sleep, daytime fatigue, and even cardiovascular issues.
In this article, we will explore how enlarged tonsils contribute to sleep apnea, identify the symptoms associated with this condition, and discuss the methods used for diagnosing tonsil-related sleep apnea.
How Enlarged Tonsils Contribute to Sleep Apnea
Enlarged tonsils can significantly obstruct the airways during sleep, leading to sleep apnea. This obstruction occurs because the tonsils are located on either side of the throat, and when they become swollen, they can block the passage of air. This is particularly problematic during the deeper stages of sleep when muscle tone decreases, causing the airway to collapse more easily.
In children, enlarged tonsils are one of the most common causes of obstructive sleep apnea. Studies have shown that tonsillectomy, the surgical removal of the tonsils, can effectively alleviate sleep apnea symptoms in many pediatric cases. This highlights the importance of early diagnosis and treatment to prevent long-term health issues.
In adults, the situation can be more complex as other factors such as obesity, nasal congestion, and anatomical variations can also play a role. However, when enlarged tonsils are identified as the primary cause, they contribute to the repetitive pauses in breathing that characterize sleep apnea, leading to fragmented sleep and oxygen desaturation.
Symptoms of Enlarged Tonsils
Recognizing the symptoms of enlarged tonsils is the first step in identifying potential sleep apnea. Common symptoms include:
- Chronic snoring
- Frequent pauses in breathing during sleep
- Restless sleep or frequent awakenings
- Daytime fatigue or excessive sleepiness
- Difficulty swallowing or sore throat
- Recurrent throat infections
In children, enlarged tonsils can also lead to behavioral issues such as hyperactivity, attention deficits, and poor academic performance due to the lack of restful sleep. If these symptoms are present, it is essential to seek medical advice as early intervention can prevent more serious complications.
Diagnosis of Tonsil-related Sleep Apnea
Diagnosing tonsil-related sleep apnea involves several steps. Initially, a detailed medical history and physical examination are conducted. The doctor will look for signs of enlarged tonsils and inquire about sleep patterns, snoring, and daytime symptoms.
In many cases, a sleep study, or polysomnography, is recommended. This test monitors various physiological parameters during sleep, such as brain activity, eye movements, heart rate, and oxygen levels. It provides comprehensive data to confirm the presence and severity of sleep apnea.
For children, a simpler overnight pulse oximetry test may be used to measure oxygen levels during sleep. If the results indicate frequent drops in oxygen saturation, this may suggest sleep apnea related to enlarged tonsils.
Once diagnosed, the treatment plan may include surgical options such as tonsillectomy or other interventions such as continuous positive airway pressure (CPAP) therapy. Early and accurate diagnosis is crucial for effective treatment and can significantly improve the quality of life for patients suffering from sleep apnea.
In conclusion, understanding the role of enlarged tonsils in sleep apnea is essential for proper diagnosis and effective treatment. If you found this article helpful, consider reading our other articles on sleep disorders and their various treatment options to gain more insight into maintaining good sleep hygiene and overall health.
Prevention and Management of Sleep Apnea
Sleep apnea is a serious sleep disorder characterized by repeated interruptions in breathing during sleep. The two main types of sleep apnea are obstructive sleep apnea (OSA) and central sleep apnea (CSA). The prevention and management of sleep apnea involve a multidisciplinary approach that includes lifestyle modifications, medical interventions, and surgical treatments. This article will explore evidence-based strategies for preventing and managing sleep apnea.
Proper management of sleep apnea is crucial because untreated sleep apnea can lead to significant health complications like cardiovascular diseases, stroke, diabetes, and daytime fatigue. Management typically begins with lifestyle changes and progresses to medical and surgical interventions if necessary. Early diagnosis and a tailored treatment plan can significantly improve the quality of life for individuals suffering from sleep apnea.
Lifestyle Changes
Implementing lifestyle changes can be a highly effective first step in managing mild to moderate sleep apnea. Weight loss, for instance, has been shown to significantly reduce the severity of obstructive sleep apnea. Excess weight, particularly around the neck, can obstruct the airway, and losing weight can help alleviate this obstruction.
Another crucial lifestyle change is adopting a regular sleep schedule. Good sleep hygiene can include going to bed and waking up at the same time every day, avoiding caffeine and heavy meals before bedtime, and creating a comfortable sleep environment. These habits can help ensure that sleep is restful and uninterrupted. Positional therapy can also play a role in managing sleep apnea. Many individuals with OSA experience more frequent episodes when sleeping on their back. Using positional devices or special pillows to encourage side-sleeping can reduce the frequency of apnea events. Additionally, avoiding alcohol and sedatives, which can relax throat muscles and worsen sleep apnea, is advisable.
Medical Interventions
When lifestyle changes are not sufficient, medical interventions often become necessary. Continuous Positive Airway Pressure (CPAP) therapy is the most commonly prescribed treatment for moderate to severe obstructive sleep apnea. CPAP machines work by delivering a continuous stream of air through a mask, which keeps the airway open during sleep. This intervention has been well-studied and is highly effective in reducing apnea episodes.
Oral appliances are another option for managing sleep apnea. These devices, similar to mouthguards, reposition the lower jaw and tongue to keep the airway open. They are particularly effective for individuals with mild to moderate OSA and are often recommended for patients who cannot tolerate CPAP therapy.
In some cases, medications may be prescribed to manage underlying conditions contributing to sleep apnea. For example, individuals with central sleep apnea may benefit from medications that stimulate breathing. However, medication is generally considered a supplementary treatment rather than a primary method of management.
Surgical Treatments
Surgical treatments are usually considered when other interventions have failed or when there is an anatomical reason for the airway obstruction. Uvulopalatopharyngoplasty (UPPP) is a common surgical procedure that removes excess tissue from the throat to widen the airway. This can be effective in reducing or eliminating sleep apnea episodes.
Another surgical option is maxillomandibular advancement (MMA), which repositions the jaw to enlarge the space behind the tongue and soft palate, thus reducing airway obstruction. This procedure is more invasive but can be very effective for severe cases of sleep apnea.
For patients with nasal obstructions contributing to sleep apnea, surgeries such as septoplasty or turbinate reduction may be recommended. These procedures aim to improve airflow through the nasal passages, making breathing easier during sleep.
Advances in surgical techniques and technologies continue to provide new options for individuals suffering from sleep apnea. However, it is essential to consult with a healthcare provider to determine the most appropriate treatment plan based on individual circumstances.
Interested in learning more about sleep disorders and their treatments? Read our other articles to explore further insights and expert advice.
Understanding the Link Between Tonsils and Sleep Apnea
If you suffer from disrupted sleep, your tonsils may play a bigger role than you realize. Here’s a look into how tonsils can impact sleep apnea.
How do tonsils affect sleep apnea?
Tonsils can affect sleep apnea primarily when they are enlarged, a condition known as tonsillar hypertrophy. Enlarged tonsils can obstruct the airway during sleep, reducing airflow and leading to sleep apnea symptoms such as snoring and intermittent breathing pauses. Removal of enlarged tonsils, through a procedure known as tonsillectomy, is often recommended to alleviate these symptoms and improve nighttime breathing.

My name is Salman Kapa, a 73-year-old expert in bone regeneration and dental implantology. With decades of experience in the field, I am dedicated to advancing our understanding of oral health and hygiene. Through my research and writing, I aim to contribute to the development of innovative solutions in dental care.




